Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
VA »
Health Care »
Geriatric Research Education and Clinical Center (GRECC)
»
Fall 2024 GRECC Forum on Aging
Geriatric Research Education and Clinical Center (GRECC)
Fall 2024 GRECC Forum on Aging
GRECC Director's Message
 As always, it is a pleasure to share news and updates in clinical innovation, education, and research in aging produced by the GRECC workforce at our twenty sites across the country.
As always, it is a pleasure to share news and updates in clinical innovation, education, and research in aging produced by the GRECC workforce at our twenty sites across the country.
With every issue of the Forum, we look back on the previous two quarters and highlight the output of our GRECCs in each of its three missions. In this issue’s feature article, however, we have the opportunity to take an even longer view by describing the findings of a recently published manuscript that quantifies the breadth and depth of GRECC accomplishments in a recent five-year period. This being both the start of the fiscal year and the 50th anniversary of the GRECC’s existence, I can think of no better way to find inspiration for the days ahead than to celebrate all that our GRECC staff have already done to move the care of aging Veterans forward.
Improving care for aging Veterans remains at the heart of the VA Age-Friendly initiative, as well, and in this issue, we introduce the new Age-Friendly Community housed on the VA Diffusion Marketplace website. We also showcase the national reach of VA Age-Friendly programs through features on the IHI website and in high-impact publications. In each instance, our VA providers demonstrate the meaningful outcomes that Age-Friendly health care offers to both individual Veterans and the health systems that support them.
Other items in this edition include the development of a new mouse model for sarcopenia, an intriguing connection between Agent Orange exposure and lower urinary tract symptoms, better management of chronic pain in people with HIV through self-management and peer support, enhancement of psychiatric care for older Veterans through the Geriatric Scholars Program, more efficient medication management through a VA-based home visit program, clearer documentation of key partners involved in Veterans’ care, and much more. Many thanks to all those who contributed their stories to this issue and cheers to another 50 years of GRECC achievements!
Please enjoy this issue of Forum on Aging and feel free to share with others.
Marianne Shaughnessy, PhD, CRNP
Director GRECC Programs
FEATURE ARTICLE
GRECC Directors Association Manuscript Highlights Five Years of Collective Accomplishments in Research, Education, and Clinical Innovation
Through research, education, and innovation in clinical care, the nation’s 20 GRECCs have spent nearly 50 years seeking to improve the lives of aging Veterans everywhere. GRECC staff spend much of their time looking ahead, anticipating the challenges of caring for a growing population of older Veterans and creating novel ways to ensure the VA system rises to meet those challenges now and in the future. Recently, however, lead author, Dr. Timothy W. Farrell, and GRECC colleagues took an opportunity to look back, describing how far these efforts have moved forward not only Veterans care but that of the general public in recent years. 
The resultant manuscript entitled “Impact of Veterans Affairs Geriatric Research, Education, and Clinical Centers: Incubators of innovation in geriatrics,” was published in the Journal of the American Geriatrics Society. Along with co-authors, Taissa Bej, Pamela Flinton, and Drs. Beth Hogans, Robin Jump, Alayne Markland, Cathy Alessi, Steven Barczi, Robert Bonomo, Jorie Butler, G. Paul Eleazer, Randall Rupper, Mark Supiano, Marianne Shaughnessy, Dr. Farrell examined GRECC data from 2018 through 2022 to measure the innumerable impacts of GRECCs both within and outside the VA. The authors reviewed each arm of the GRECC mission, showcasing highlights and quantifying the ways in which GRECCs have made an impact.
Beginning with the output of GRECC investigators, the authors described the volume of research, noting that several thousand manuscripts had been published by GRECC authors in the examined time period. They also reviewed the impressive breadth of expertise of GRECC scientists, who conduct investigations in “biology of aging and healthy aging; Alzheimer's disease and related dementias; physical exercise and exercise interventions; and geriatric syndromes and age-related medical conditions,” as well as “dissemination and implementation science methodologies.” The work of GRECC scientists has seen growing financial support, too, with an increase of expenditures by $100 million between 2017 and 2022. The paper further detailed several high impact publications and presented data regarding the significant annual citation rates of papers written by GRECC investigators. The calculated h-index, a measure of research and publication output where higher numbers are better and 60 is considered “exceptional”, is 135 for the GRECC manuscripts, highlighting the immense productivity and impact of GRECC researchers.
Dr. Farrell and colleagues went on to review the contributions of GRECC educators. The GRECC education mission is broad in scope and includes not only trainees but also VA clinicians, Veterans, and those who care for Veterans. This, the authors concluded, results in more than 250,000 person-hours of education annually across all sites. With a strong interprofessional focus for education, GRECCs were found to reach 15 different health professions, including physicians, nurses, dentists, pharmacists, social workers, clinical psychologists, chaplains, registered dieticians, physical, occupational, speech and language therapists, and recreational therapists, audiologists, optometrists, and podiatrists. The manuscript further described the numerous programs devoted to educating practicing clinicians in the VA, from the many iterations of the successful Geriatric Scholars Program, to GRECC Conn etc. webinars and the Aging and Cognition Education Workgroup. It also covered the educational products aimed at Veterans and their care partners – face to face groups, workbooks and booklets, and virtual resources that are available 24-7 whenever they are needed. As noted by the authors, GRECCs have made an enormous impact on education over the five years studied and will continue to lead the way going forward.
Finally, the authors detailed the clinical innovations that have kept the VA ahead of the curve through targeted interventions that benefit aging Veterans. They featured nine nationally disseminated projects that have been widely adopted and have yielded meaningful outcomes for Veterans. Among the programs they highlighted, Coordinated Transitional Care (C-TraC) has spread to numerous other VA settings and beyond and has been shown to reduce unplanned 30-day hospital readmissions by one-third through a structured, telephone-based nursing intervention (Kind AJH Health Affairs (Millwood) 2012). Gerofit, another nation-wide intervention that got its start as a GRECC Clinician innovation, has shown a 25% lower 10-year mortality rate among participating Veterans who engage in its structured exercise programs (Morey MC Journal of the American Geriatrics Society, 2002). A third program, STRIDE reduced the chances of skilled nursing facility discharge by 40% at a low cost by offering hospitalized Veterans opportunities for supervised walking to maintain their strength (Hastings SN Annals of Internal Medicine, 2023). The authors discussed that these programs not only benefit Veterans but have also raised the standards for quality of care among older adults outside the VA system, as well.
Dr. Farrell and his colleagues concluded that certain qualities of the VA GRECCs make the model uniquely suited to innovate and disseminate and function as a so-called “incubator” for new ideas in geriatrics. The existence in a capitated health care system provides flexibility when creating new clinical programs that are not bound by the traditional fee for service model, and the national reach allows for rapid adoption of effective care models across the country. The VA’s immense educational footprint provides fertile ground for cultivating the next generation of geriatrics-minded health care professionals who can spread VA-developed best practices far and wide. What is more, the close connection between research, education, and clinical care moves novel ideas from the bench to the bedside efficiently and effectively. As the authors looked back on a remarkably productive five years of GRECC efforts, they also chart a path forward for health care by showing the critical role GRECCs play and the potential they have to shape the future of care for the aging population.
Contact: Elizabeth.Chapman3@va.gov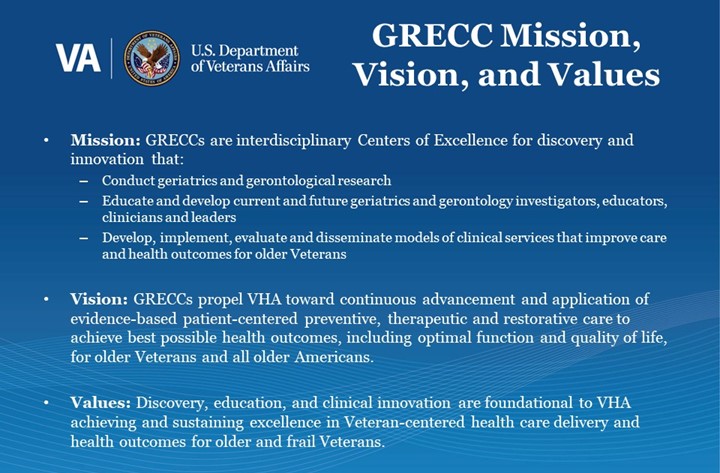
AGE-FRIENDLY
VA Age-Friendly Community Now Featured on Diffusion Marketplace
Joining VA Immersive and Suicide Prevention, the Age-Friendly Health Systems now has its own community on the VA Diffusion Marketplace. The Age-Friendly Community offers the latest news, publications, and resources for sites that want to get started on their journey. It also features a variety of exemplar innovations that support Age-Friendly care, such as Gerofit, STRIDE, VIONE and The Surgical Pause. Visitors can find a listing of upcoming and past events as well as blog posts and other media related to Age-Friendly Health Systems in VA. Visitors will also find a list of recent publications arising from VA Age-Friendly interventions that show the measurable, positive impact this initiative is having on Veterans.
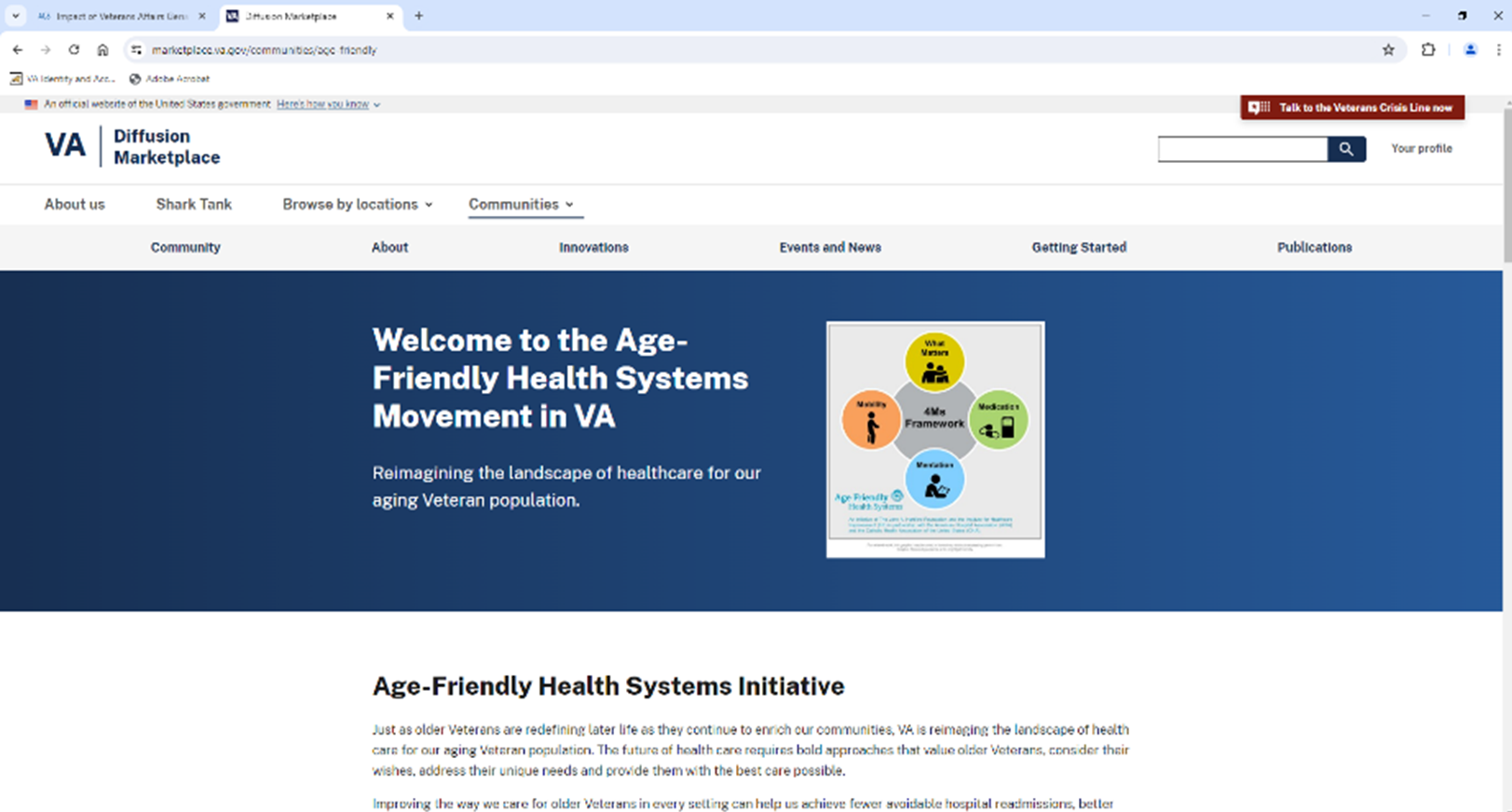
VA Age-Friendly Champions Featured on IHI Blog
The VA is home to many clinicians and programs that serve as models for how to embrace the 4Ms and make meaningful differences in the care of older adults. The Institute for Healthcare Improvement (IHI) recently featured Dr. Laurence Solberg, Associate Director for Clinical Innovation at the Gainesville GRECC, in a blog post. Dr. Solberg shares how the Gainesville Community Living Center helped a Veteran find the motivation to get through rehabilitation and back home by asking what matters most. Dr. Solberg also discussed how his facility’s Age-Friendly efforts allowed him and his colleagues to align the work they were already doing within the 4Ms framework and link it to what matters most to the Veterans they serve.
In another IHI blog feature, Dr. Shivani Jindal, Director of Transition of Care for the Cincinnati VA Medical Center and a physician who provides in-home visits for Veterans as part of Hospital in Home, explained how the 4Ms have enhanced both her care of Veterans and the way she teaches trainees. In the post, Dr. Jindal describes a breakthrough in her care of a Veteran who was having difficulty adhering to his diuretic regimen that resulted from taking the Age-Friendly approach. She credited the 4Ms, specifically asking what matters most, with allowing her to practice empathy and connect with the Veterans she serves. She also emphasizes how the 4Ms framework gives structure to her team huddles, visits with patients, documentation of encounters, and the teaching she provides to the interprofessional trainees who she precepts.
Dr. Jindal’s and Dr. Solberg’s stories and accompanying videos can be found in the News section of the Age-Friendly Community on the Diffusion Marketplace.
VA Boston and New England GRECC Staff Connect Age-Friendly Efforts to Improvements in Outcomes for CLC Veterans
Investigators from the Boston VA Healthcare System and New England GRECC recently analyzed the impact of Age-Friendly implementation on clinical and quality outcomes in a VA Community Living Center and found significant benefits. In a manuscript published in the Journal of the American Geriatrics Society (King SE Journal of the American Geriatrics Society, 2024), the team detailed how becoming Age-Friendly led to safer prescribing practices, fewer falls and disruptive behavior reports, and improved documentation of what matters to Veterans. The authors also discovered that Age-Friendly implementation reduced rehospitalizations, decreased emergency department utilization, and improved patient satisfaction. A link to the manuscript, written by Sarah E. King MD, Marcus D. Ruopp MD, Chi T. Mac PharmD, Kelly A. O'Malley PhD, Jordana L. Meyerson MD, MSc, Lindsay Lefers PT, DPT, Jonathan F. Bean MD, MPH, Jane A. Driver MD, MPH, and Andrea Wershof Schwartz MD, MPH, AGSF, is located in the Publications section of the Age-Friendly Community on the Diffusion Marketplace.
Contact: AgeFriendly@va.gov
RESEARCH
GRECC Scientists Help Link Agent Orange Exposure to Lower Urinary Tract Symptoms
Steven C. Castle, M.D. and collaborators Abigail Viado, Anne R. Griffin, RN, MS; Frank Catapano, and Cathy C. Lee, M.D. were studying the effect of Agent Orange Exposure (AOE) on mobility and balance when they noticed a curious trend: many Veterans with presumed AOE also had overactive bladder symptoms (OAB) or Lower Urinary Tract Symptoms (LUTS).
Their Clinical Innovations Project is funded by the National Office of Geriatrics and Extended Care and aims to understand health impacts of Agent Orange, the herbicide containing Dioxin that 2.7 million US Military may have been exposed to between 1962-71. It is estimated that over 300,000 US Veterans and over 400,000 Vietnamese individuals died from AOE between 1962 and 1971, and AOE has been tied to an increase in healthcare utilization due to a number of conditions, including leukemia, lymphoma, prostate and other cancers, type 2 diabetes mellitus, ischemic heart disease, Parkinson’s Disease, and more. Until now, however, there was no connection between AOE and urinary symptoms.
A literature search did not identify any human studies or reports connecting AOE to bladder symptoms, but three rodent studies suggested an association between fetal or neonatal exposure to the substance and dysfunction of the lower urinary tract in adulthood. The studies also showed differences in the microscopic structure of bladders, bladder mass, and urodynamic voiding behavior in exposed rodents (Ricke WA 2016, Turco AE 2021). This encouraged Dr. Castle and colleagues to look deeper into the connection between urinary symptoms and AOE.
Their existing project had already adopted qualitative and quantitative tools to measure AOE risk. With input from Atlanta/Birmingham GRECC experts in LUTS, they selected the Lower Urinary Tract Symptom Index-10 (LURN SI-10) to screen for LUTS among Veterans. They then compared the LURN SI-10 scores of three groups:
- Negative Presumed AOE (Qualitative and Quantitative scores = 0)
- Presumed AOE (Qualitative AND Quantitative AOE risk questionnaires both >0)
- Presumed AOE (Qualitative OR Quantitative >0)
Ultimately, 25 Vietnam Veterans were surveyed with the LURN SI-10. They found significantly lower LURN SI-10 scores in Veterans with negative Qualitative AND Quantitative AOE risk compared to Veterans with presumed AOE (see Figure).
The investigators concluded that AOE/Dioxin Exposure among Veterans may have a lasting impact on the bladder, causing LUTS that are similar to Overactive Bladder. Going forward, the investigators will begin teaching affected Veterans pelvic floor strengthening exercises and monitoring LURN SI-10 scores for improvement. Failing that, the group intends to place a referral to Urology for a possible medication trial.
Contact: Steven.Castle@va.gov
Promoting Self-Management and Peer Support Among Adults with HIV and Chronic Pain
Older adults represent a growing population of people with HIV (PWH). Aging with HIV can bring with it a host of challenges, including age-related changes that can be exacerbated by chronic pain, such as falls. Attention to chronic pain in older adults with HIV is especially important given the high prevalence of co-occurring substance use and geriatric conditions, making opioid and other pharmacologic treatments risky.
Dr. Katie Fitzgerald Jones, a Nurse Scientist in the New England GRECC at VA Boston Healthcare System, and her colleagues tested an innovative pain self-management intervention, called Skills TO Manage Pain (STOMP). The STOMP intervention delivers peer support provided by a person with HIV who has strong pain management and communication skills and is coupled with 1:1 pain self-management education delivered by clinical staff typically found in HIV clinics (social workers or health coaches). The intervention was tested in a multisite randomized control trial, and the results demonstrated a clinically significant improvement in pain in the STOMP group compared to enhanced usual care. Dr. Jones notes, “We are excited about the findings. The difference of > 1 point on a 0-10 pain scale is, for many patients, a difference between being able to go to the grocery store, do laundry, or attend a grandchild’s basketball game.”
The primary outcome paper is featured in JAMA Internal Medicine and was presented at the International AIDS Impact in Stockholm, Sweden, in 2023. The study findings and publication received attention from Healio and Medpage Today and was named the top paper of the week by the International Association for the Study of Pain.
The study findings underscore that peer support and pain self-management education are essential to coping with chronic pain. Dr. Jones said, “We are fortunate that pain self-management tools and peer navigators are readily available within the VA Whole Health program. However, an important aspect of pain self-management education is tailoring to unique biopsychosocial factors associated with a given condition.” Foundational work by the study PI Jessica Merlin at the University of Pittsburgh demonstrated that people with HIV and chronic pain face stigma, high rates of opioid use, and communication challenges with clinicians.
Dr. Jones’ preliminary work demonstrates similar challenges in cancer survivors, another older adult population with a high prevalence of chronic multisite pain (Jones KF, Journal of Hospice & Palliative Nursing 2023), opioid use (Jones KF, Journal of Pain and Symptom Management 2021) and communication challenges (Jones KF, Journal of Palliative Medicine 2023). Moreover, the VA has been a leader in testing peer-support interventions for chronic pain (Matthias MS, Journal of General Internal Medicine 2020). Dr. Jones and the team hope to adapt and test STOMP in other populations, including Veteran cancer survivors with STOMP intervention, providing an essential blueprint.
Contact: Katie.Jones4@va.gov
GRECC Scientists Use Novel Sarcopenia Definition in Mice to Expand Understanding of Underlying Mechanisms
Many older Veterans lose muscle mass and function as they age, a condition called sarcopenia. In addition to being linked with frailty, higher mortality, and lower quality of life, sarcopenia is associated with falls, cardiac disease, respiratory disease, and cognitive impairment. While the consequences of sarcopenia are substantial, less is known about how sarcopenia develops on the cellular and molecular levels. With the ultimate goal of finding future therapeutic targets, Dr. Jose Garcia, Dr. Haiming L. Kerr, and other colleagues from the Puget Sound VA GRECC collaborated to create a better model of sarcopenia in older mice. This model allowed them to understand the relationship between the loss of muscle mass and declines in muscle function better and also provided new insight into to molecular mechanisms underlying the progression of sarcopenia and how they may differ by sex.
In their most recent publication in the Journal of Clinical Investigation, the scientists describe this work, including how they improved identification of sarcopenia in mice by using criteria that match elements used to define the condition in humans. Whereas previous rodent-based studies had used older age as the sole criterion for sacropenia and employed mice equivalent to 56 – 69-year-old humans, this investigation aimed to be more precise. In addition to using mice that were older, they designated mice as definitely sarcopenic only if they were also two standard deviations below the mean of young, healthy mice in assessments of function (grip strength and treadmill running time) and muscle mass. This resulted in between 9-22% of older male mice meeting the cut-offs for definite sarcopenia. Interestingly, female mice had a lower incidence of definite sarcopenia compared to males, but they had more cases of mice with decreased muscle function only, deemed “probable sarcopenia”.
Equipped with this enhanced model, they observed key changes in muscles over time when comparing older mice with sarcopenia to those without. In general, they found that sarcopenic mice had more dramatic decreases in muscle function than in muscle mass and that sarcopenic male mice had decreased muscle contractility. They also noted a trend toward lower type IIB fiber size. On the cellular level, they found that this correlated with decreased mitochondrial biogenesis and oxidative capacity. They identified molecular differences as well, with AMPK-autophagy signaling significantly lower in male mice with sarcopenia, while pathways linked to mitochondrial metabolism positively correlated with muscle mass. Notably, they did not observe these differences in female mice.
When reflecting on the findings, Dr. Kerr commented, “Our study offers a practical definition of sarcopenia in mice that is highly relevant to humans. We demonstrate how muscle mass and function decline at different rates as mice age, and we highlight the distinct effects of aging and sarcopenia on key molecular markers. Our research provides valuable insights into the underlying mechanisms of sarcopenia and establishes a foundation for future studies to develop novel therapeutic targets for this condition.”
Those interested in reading further details about this investigation can find the manuscript, titled “Mouse Sarcopenia Model Reveals Sex- and Age-Specific Differences in Phenotypic and Molecular Characteristics,” in the Journal of Clinical Investigation. Co-authors include: Haiming L. Kerr, PhD; Kora Krumm, MS; Barbara Anderson, MS; Anthony Christiani, BS; Lena Strait, BS; Theresa Li, BS; Brynn Irwin, BS; Siyi Jiang, BS; Artur Rybachok, BS; Amanda Chen, BS; Elizabeth Dacek, BS; Lucas Caeiro, MD; Gennifer E. Merrihew, MS; James W. MacDonald, PhD; Theo K. Bammler, PhD; Michael J. MacCoss, PhD; and senior author, Jose M. Garcia, MD, PhD. It is also accompanied by a video abstract featuring Drs. Garcia and Kerr describing their novel findings.
Contact: Haiming.Kerr@va.gov
EDUCATION
Enhancing geriatrics competencies for psychiatric care providers
The VA faces widespread geriatric workforce shortages that mirror those seen in the US at large. In recognition of the need to enhance healthcare for older Veterans, the VA has invested in developing the skills for its primary care workforce through the Geriatric Scholars Program (GSP).
Launched in 2008 with funding from the VHA Offices of Rural Health and Geriatrics and Extended Care, the GSP has expanded over the years with programs for multiple disciplines including primary care providers, pharmacists, psychologists, social workers, and rehabilitation therapists. A recent addition is the GSP for psychiatric providers. Piloted regionally in VISN8, 2024 marked the third installment of the Psychiatry track. Educational leaders from several GRECCs collaborated with a multidisciplinary team of experts to develop this curriculum. To date, 40 psychiatric care providers have participated in the program including psychiatrists, nurse practitioners and physician assistants.
At the core of this longitudinal program is an intensive 4-day course on Geriatric Psychiatry paired with a 1-day quality improvement (QI) training. Following this intensive, scholars initiate a local QI project aimed at improving psychiatric care of older Veterans. The curriculum for the 4-day course covers three broad areas: 1) general topics in geriatrics such as the comprehensive geriatric assessment, sensory impairment and communication with older adults; 2) core topics in geriatric psychiatry such as neurocognitive disorders, anxiety, PTSD, depression, substance use, pain and sleep disturbances; and 3) specialty topics such as end-of-life considerations, caring for diverse population, and sexuality in aging.
During the QI Day, participants are introduced to basic QI principles such as Plan-Do-Study-Act (PDSA) cycles, SMART goal statements, and the fishbone diagram for root cause analysis. They also learn how to use VA resources and data sets. Over the next 6 months they periodically meet with their assigned QI mentor who guides them through the implementation of their project.
The psychiatry track curriculum was developed using adult learning principles and includes a strong case-based component that fosters clinical reasoning and group discussion. Each day begins with a case presentation and ends with the case analysis. Throughout the training, both presenters and participants bring in challenging patient cases from their personal practice for discussion. Although the 5-day program was delivered virtually on Teams, organizers were able to incorporate experiential learning activities (see Figure) and witnessed a high level of interaction among participants with active discussions and sharing of resources via the chat box.

Figure: Experiential activity related to sensory impairment: “Can you manage your medications? Identify the GREEN pills. We have given you a little ‘yellowing of the lens.’”
The program evaluation showed a high level of participant satisfaction with the presenters and the content covered as well as enhanced competence. Feedback from participants shows they especially valued the interactions with the presenters and their peers, the clinical applicability of the case discussions, and the diversity of topics covered. They also noted that the QI training put some of their initial anxieties surrounding the QI project to rest. Examples of QI projects include “Measurement of loneliness in geriatric Veterans with severe mental illness”, “Management of dementia with behavioral disturbances in the hospital setting.” and “Anxiety screening in older Veterans.”
The GSP team welcomes the 2024 cohort to the growing team of change agents at the VA as they continue to empower our existing workforce and equip them with the knowledge and skills to provide high-quality mental health care to our aging Veteran population. The Geriatric Psychiatry Scholars program was recently featured during a Geriatric Education Paper Session at the 2024 American Geriatrics Society’s annual meeting.
The GSP team thanks its collaborators, including: Rose Maria van Zuilen, PhD (Miami GRECC/University of Miami); Carmen Fernandez, PsyD (Gainesville GRECC); Sarah Hyduke, MSW, Josie Kramer, PhD, and Luis Melendez, MPA (Geriatric Scholars Program/LA GRECC); Rachel Rodriguez, PhD (Durham GRECC); Carol Callaway-Lane, DNP and team (VA Quality Scholars Program); Josepha Cheong, MD (Gainesville GRECC); Michele Karel, PhD (VHA Geriatric Mental Health); Samer Nasr, MD and Carri-Ann Gibson, MD (VISN 8); and the rest of our outstanding team of planning committee and faculty members.
Contact: Carmen.Fernandez2@va.gov
Bronx GRECC Highlights 4Ms of Age-Friendly Health Systems
On September 19th, the VISN 2 GRECC, located at James J Peters VA Medical Center (VAMC) in Bronx, NY held its 4th Annual VISN 2 GRECC Virtual Webinar: Updates in Geriatrics and Palliative Care. The annual event is held in collaboration with innovative providers across the New York/New Jersey region and the nation, with the goal of educating VA providers about best practices in geriatrics and palliative medicine.
 This year's webinar spotlight was Age-Friendly Health Systems, which is a top priority of VA. In 2020, the Veterans Health Administration pledged to become the largest integrated health system to be recognized as an Age-Friendly Health System in the United States (Kalsy et al, 2023). Age-Friendly Health Systems is an initiative to provide optimal care for the growing population of adults over the age of 65 by encouraging health care facilities to reliably provide four evidence-based elements of high-quality care, known as the “4Ms”: What Matters, Mentation, Mobility and Medication (Institute for Health Improvement, 2024). What Matters represents the importance of aligning a patient’s care with their personal health care goals and the patient’s values. Mentation emphasizes the need to screen for mind and mood changes that could be related to dementia and delirium. Mobility reflects safe movement to maintain function and perform activities that are important to a patient. Lastly, Medication promotes that any medications prescribed should not interfere with What Matters to a patient or their Mobility and Mentation.
This year's webinar spotlight was Age-Friendly Health Systems, which is a top priority of VA. In 2020, the Veterans Health Administration pledged to become the largest integrated health system to be recognized as an Age-Friendly Health System in the United States (Kalsy et al, 2023). Age-Friendly Health Systems is an initiative to provide optimal care for the growing population of adults over the age of 65 by encouraging health care facilities to reliably provide four evidence-based elements of high-quality care, known as the “4Ms”: What Matters, Mentation, Mobility and Medication (Institute for Health Improvement, 2024). What Matters represents the importance of aligning a patient’s care with their personal health care goals and the patient’s values. Mentation emphasizes the need to screen for mind and mood changes that could be related to dementia and delirium. Mobility reflects safe movement to maintain function and perform activities that are important to a patient. Lastly, Medication promotes that any medications prescribed should not interfere with What Matters to a patient or their Mobility and Mentation.
The VISN 2 GRECC chose the topic of Age-Friendly Health Systems to encourage other regional and national facilities to become Age-Friendly, as well as to highlight VISN 2's ongoing efforts. As of July 2024, VISN 2 had 25 Age-Friendly Health System participants, recognized as integrating evidence-based interventions around the 4Ms into their care for older Veterans (Institute for Health Improvement, 2024).
Webinar attendees were welcomed to the session by Dr. Donald A. McDonald, Deputy Chief Medical Officer for the New York/New Jersey VA Health care network, Dr. Abigail Baim-Lance, Research Health Science Specialist and Acting Associate Director, Education & Evaluation at the VISN 2 GRECC, and Dr. William Hung, VISN 2 GRECC Director. The Webinar held four presentations, one on each of the 4Ms of age-friendly care.
Dr. Angela Catic from the Houston VAMC presented on What Matters by speaking about Patient Priorities Care, a preferred framework for eliciting and aligning patient care with patients’ values. Jacquelyn Claude and Dominique Gilliam, both from the Hampton VAMC, discussed Mentation and addressed reducing social isolation through engagement and consistent assignments. Dr. Marcus Ruopp from the VA Boston Healthcare System presented on Mobility and provided a comprehensive overview of the topic. Dr. Saraswathy Battar from the West Palm Beach VA Healthcare System and Dr. Jason Corbo from the South Texas VA Healthcare System ended the day with the topic of Medication, discussing medication optimization. Each presentation was followed by a Q&A session to give attendees a chance to further learn from the speakers.
This webinar had more than 140 people register. Additionally, the Webinar session was recorded and will be processed for placement on TMS as an Enduring Asynchronous Learning item with continuing education credits. The recording and placement onto TMS will take about 90 days to complete from the date of the session.
Contact: Eugenia.Dorisca@va.gov and Lauren.Hall5@va.gov
GRECC-Based Transition to Practice Rotation Sets up Geriatrics Fellows for Success
While Geriatric Medicine fellowship programs cover a wide range of content to ensure that trainees develop the knowledge, skills, and attitudes necessary to care for complex older adults, curricula to address the day-to-day practicalities of work as an attending geriatrician after training are often lacking. Geriatric Medicine fellows rotating in the Madison VA GRECC expressed interest in a rotation that would help prepare them for the clinical pace and administrative responsibilities they would face as they started independent practice.
Fortunately, the GRECC is uniquely positioned to meet this need. Its education mission to train a prepared and competent geriatrics workforce facilitates development of innovative curricula, and Madison VA GRECC clinician educators practice in a variety of settings. From ambulatory clinics to home-based primary care, acute care, and subacute rehabilitation in the Community Living Center (CLC), working with GRECC faculty offers the chance to tailor learning venues to fellows’ future roles, whatever they may be.
In academic year 2022-2023, the fellowship launched a GRECC-based “Transition to Practice” (T2P) rotation comprised of two weeks of rigorous clinical exposures and didactics addressing key topics otherwise not included in traditional Geriatric Medicine curricula (see figure). Fellows select a track that best approximates their future job, with most clinical experiences taking place in VA. The venues are familiar to the fellows from previous rotations, but the fellows function as “junior attendings” rather than solely as a learner. They work from an attending physician’s schedule, seeing all the patients and staffing at the end of the session rather than between encounters to encourage independent thought and problem solving. They also act as the staff for more junior learners and must aim to complete documentation and remain on time throughout the day to mimic the expectations for faculty physicians.
T2P didactics cover high-yield topics relevant to independent practice that rarely receive attention during typical clinical rotations. Among the most popular elements of the didactic curriculum is a panel of early career faculty discussing their experiences entering into practice, from searching for a job and negotiating their contracts to organizing time and developing sustainable routines. Since this type of content is missing from most fellowship and residency curricula, the session is made available to trainees in Internal Medicine residency and subspecialty fellowship programs at the institution with high levels of participation outside the Geriatrics training program.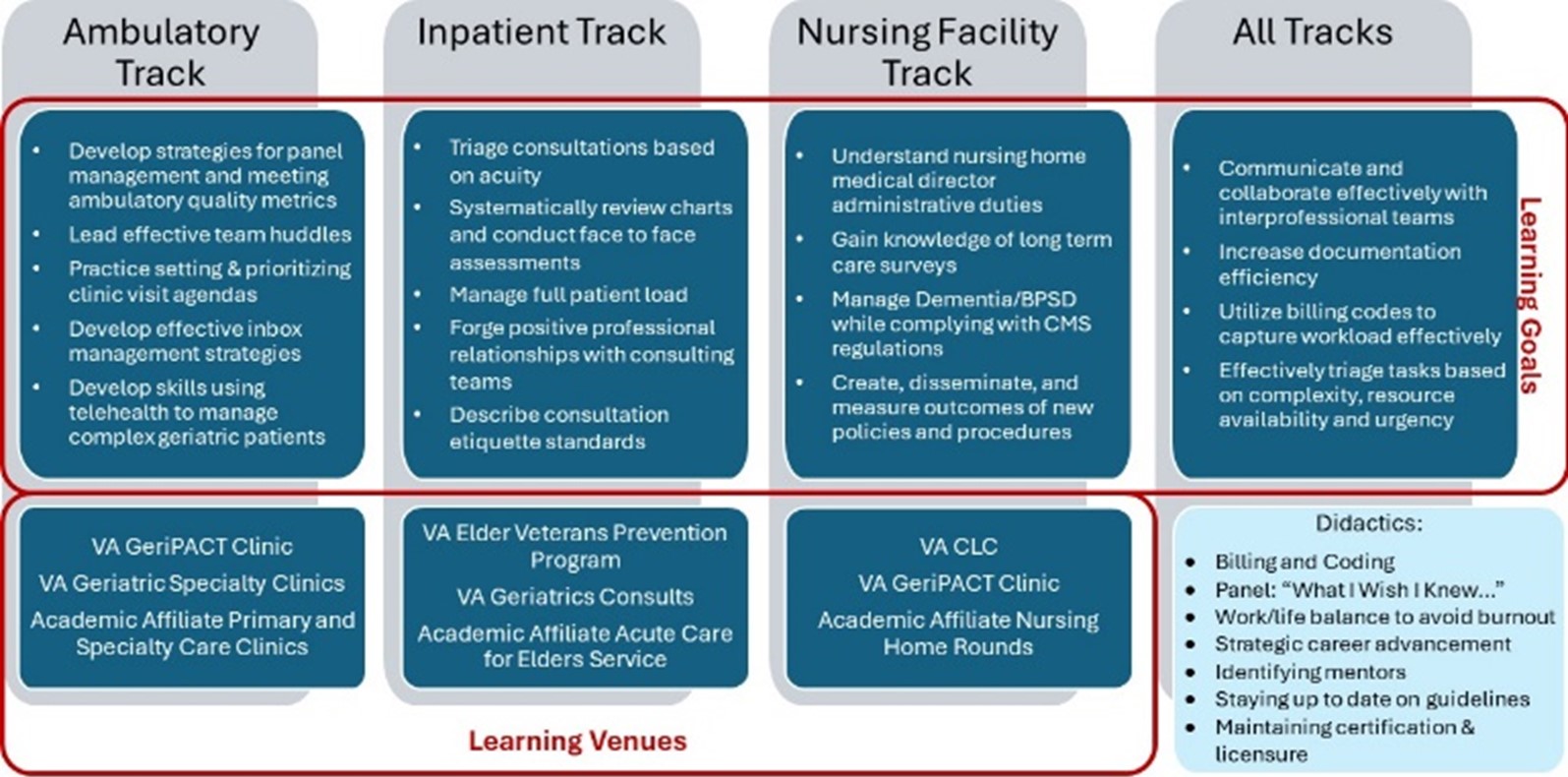
Feedback from trainees has been globally positive. Comments have included:
“The rotation gave me more autonomy with patient care than I previously had, helping me develop a mindset of independent practice before graduation.”
“I got to practice staffing patients with learners (medical students and residents) which was a skill I hadn’t had a chance to practice much in other rotations. Additionally, it was a unique rotation where I was also able to get feedback on my skills related to staffing patients with learners.”
“It was fun and refreshing to have a unique, tailored experience meant to mimic my future job. It felt like a preview of my job after graduation which made me excited and more confident to take the next step in my career.”
The program will continue this rotation going forward while collecting additional feedback to identify opportunities for improvement through rotation evaluations and graduate surveys.
Videos to prepare Older Veterans and their Care Partners for having Matters Most Conversations
What matters most to older Veterans? Each person has their own unique set of values, priorities, and health care preferences. Having conversations about what matters most is critical for guiding person-centered care plans. Yet, Veterans can be unprepared and even surprised when their health care team initiates “matters most” conversations. To provide important context for these discussions, our team created 4 short video vignettes, each illustrating how different Veteran-identified goals can guide different types of care plans.
What are the videos about? Each story features an actor playing the role of an older Veteran who is able to work toward a “matters most” goal after having a conversation with his/her/their healthcare team. The videos are designed to be shared directly with older Veterans and their care partners. If you would like to share information about how to access these videos with patients and their care partners directly, feel free to use this one-page handout or this trifold flyer, which have been approved by the Public Affairs Officer at VA Bedford.
In conceptualizing the videos, we intentionally drew from concepts central to 3 nationwide initiatives: the Age-Friendly Health Systems movement, Patient Priorities Care, and Whole Health. Age-Friendly care is built upon the “4 Ms” of Geriatrics (What Matters, Mentation, Mobility, and Medications), Patient Priorities Care presents a framework for identifying and acting on what matters to older adults by aligning care plans with their values, goals and priorities, and Whole Health is a VA approach to person-centered care for Veterans of any age using such tools as the Personal Health Inventory, Circle of Health, and the concept of a Veteran’s Mission, Aspiration and Purpose. The video descriptions that follow share a few examples of how these concepts were incorporated into the creation of the various storylines.
Meet Alex: In this story, Alex takes his dog Mugsy on regular walks around the neighborhood, until something gets in the way of Alex and Mugsy continuing the walks that they both enjoy. Click here to watch Alex’s story!
Concepts Incorporated into Alex’s Story
- Age-Friendly & Geriatrics “M” domains:
- Matters Most, Mentation
- Patient Priorities Care “One Thing:”
- To conquer his concerns about forgetting information when encountering his neighbors so that he can resume his neighborhood walks with Mugsy
- Whole Health Circle of Health Elements:
- Power of the Mind, Mindful Awareness
Meet Lillian: In this story, Lillian has recently moved in with her family, and she feels like something is missing in her new routine. Click here to watch Lillian’s story!
Concepts Incorporated into Lillian’s Story
- Age-Friendly & Geriatrics “M” domains:
- Matters Most, Multicomplexity
- Patient Priorities Care “One Thing:”
- To overcome her barrier of not being able to drive in order to travel locally during the day so that she can have more opportunities to give back to her community.
- Whole Health Circle of Health Elements:
- Personal Development, Surroundings
Meet Marty: In this story, Marty loves gardening in his backyard, but his neighbor notices he hasn’t been out in the garden much lately and goes over to find out why. Click here to watch Marty’s story!

Concepts Incorporated into Marty’s Story
- Age-Friendly & Geriatrics “M” domains:
- Matters Most, Medications
- Patient Priorities Care “One Thing:”
- To have less dizziness with position changes so that he can feel more comfortable getting back out in the garden.
- Whole Health Circle of Health Elements:
- Moving the Body, Recharge
Meet Alberto: In this story, Alberto and his wife Camila treasure being there for their granddaughter, but something is standing in the way of making it to her graduation. This video is filmed primarily in Spanish. Click here to watch a version of the video for English speakers or here for Spanish speakers.
Concepts Incorporated into Alberto’s Story
- Age-Friendly & Geriatrics “M” domains:
- Matters Most, Mobility
- Patient Priorities Care “One Thing:”
- To improve his strength and mobility so that he can make the trip to be there his granddaughter’s graduation.
- Whole Health Circle of Health Elements:
- Family, Friends & Co-workers
Who was on the video team? We assembled a VHA team of subject matter experts, spanning two GRECC sites: the New England GRECC at VA Bedford, and the Puget Sound GRECC. Multiple different professions were represented: 2 geriatric medicine physicians, a geriatric nurse (who is also a Veteran), a behavioral neurologist, a neuropsychologist, an occupational therapist, and a medical anthropologist with expertise in diversity, equity and inclusion. Subject matter experts also had experience with Age-Friendly Health Systems, Patient Priorities Care, Whole Health, and creating educational videos. We partnered with the talented video production team at the VHA Institute for Learning, Education and Development (ILEAD), as well as with clinicians at the filming location, VA Salt Lake City. Additionally, we worked with leaders and collaborators at the Age-Friendly, Patient Priorities Care, and Whole Health programs to review the video scripts and video footage. Funding for the videos was made possible by VHA ILEAD and the VHA Geriatrics and Extended Care Clinical Innovation Fund.
Video dissemination: The Matters Most videos have been posted by the Department of Veterans Affairs to its YouTube channel, and so far, these have received over 5,500 views! The videos have been shared throughout VHA at a local, regional, and national level, with dissemination avenues directed to older Veterans, their care partners, and clinicians. The videos were also circulated broadly to celebrate What Matters to You Day on June 6th 2024, via social media posts by both VA and community organizations, including the American Geriatrics Society, and the videos have reached about 27,000 views on Facebook.
We are honored to have had the opportunity to create these videos with the support of the GRECC. We believe that preparing Veterans to have matters most conversations with their healthcare teams will lead to Veterans feeling valued, cared for, and listened to, with increased satisfaction in their overall care.
Contact: Catherine.Dawson@va.gov
The Palliative Scholars Program: Enhancing Capacity to Deliver Primary Palliative Care in Interdisciplinary Trainees
Background: Evidence demonstrates the value of integration of Palliative and Supportive Care practices into the care of those with advanced and serious illness across care settings. The national workforce gap is expanding, and access to trained palliative care professionals, especially in rural communities, is largely unmet.
The Palliative Scholars program was conceptualized jointly by Dr. Sumathi Misra from the Nashville/Tennessee GRECC and Dr. Katharina Echt from the Birmingham/Atlanta GRECC in 2018 and initiated as an Advanced Practicum offering under the umbrella of the Geriatric Scholars program led by the Greater Los Angeles (GLA) GRECC. It was implemented in multiple iterations that evolved due first to COVID and then continuing funding constraints in the setting of increasing demand for palliative care practicum training by the Geriatric Scholar Alumni. This, in addition to high learner ratings, resulted in increasing requests to enroll in this opportunity to expand primary palliative care skill.
In response, Drs. Misra and Echt created an innovative blended model for FY24 to meet increased demand by the Geriatric Scholars Alumni for palliative care immersion. They piloted the concept of training interdisciplinary care team members (SW, MD, NP, PA, Pharmacy, OT, PT, Psychology) in well-established VA centers of Palliative and Supportive Care teams. The program received the highest number of requests in its history and was able to scale up and accommodate up to forty-eight scholars over six immersive sessions.
Setting and methods: Between May and August 2024, the Tennessee Valley and Birmingham/Atlanta Geriatric Research, Education and Clinical Centers collaborated to offer multiple 3-day immersive. Palliative Scholar Program practical experiences were delivered virtually to accommodate learners. Didactic learning sessions were layered on core curricular elements comprised of independent readings, web-based teaching modules, and daily live virtual case-based interprofessional clinical huddles. This created a vibrant learning community environment that allowed for didactic learning to be embedded in clinical cases. The training is personalized based on the learners’ 1) work experience in specific discipline, 2) articulated individual learning goals expressed via needs assessment, and 3) specific populations served by the trainees to enhance skill sets unique to their clinical care environment.
The program incorporates daily morning reflections and interdisciplinary team huddles via a Microsoft teams link with robust discussion of patients on the service at TVHS inpatient consult service. Multiple communication skills-based training included: (1) Simulation for experiential learning and approaches, tools and devices for accommodating sensory and cognitive aging challenges among older veterans and ensuring accessible communication among the clinical-patient-family triad; (2) Palliative Care 101; (3) Serious Illness Conversations with scripted and impromptu role play. Each day’s activities were interspersed with discipline-specific deep dives to expand interdisciplinary role appreciation and understanding of workflows with palliative social work, chaplaincy, psychology and pharmacy team members. The didactics to supplement these experiences included sessions on basic patient centered communication, prognostication, breaking bad news, goals of care discussions, pain management, integrative therapeutic approaches and procedures; integration of primary palliative care best practices into individual care setting of attendees; leadership and self-care. Multiple resources were provided on a dedicated Microsoft teams channel available as an enduring learning resource for post-practicum reference, dissemination, and integration into participants own practice and site. The practicum also includes daily debriefing Q&A and semi-structured reflective synthesis sessions by members of the group. These sessions were followed by protected time for individual self-study of curated readings, provided tools, and resources.
Post-practicum evaluation measures include assessment of factual knowledge, a combination of qualitative and quantitative data sources, a pre- and post-test, graduate follow up survey tools, and just-in-time two-way feedback loops during the immersion program.
Results: A total of 20 VA clinicians participated in one of four 3-day between May and August 2024, including social worker, physicians (Primary Care, Psychiatry, Family Medicine), physician assistants, occupational therapists, physical therapists, nurses, and pharmacists (Figure 1).
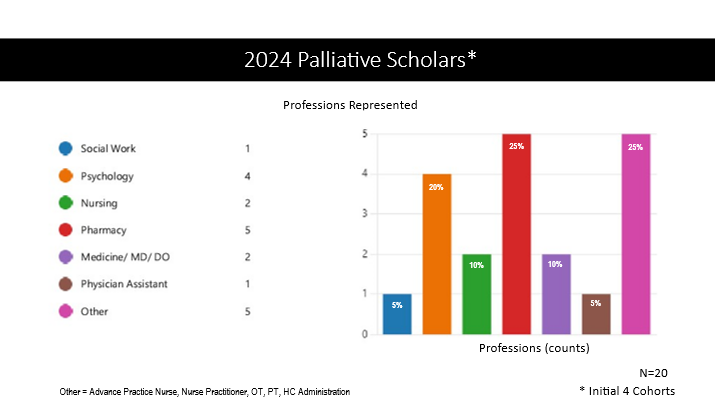
Figure 1. Palliative Scholars Professions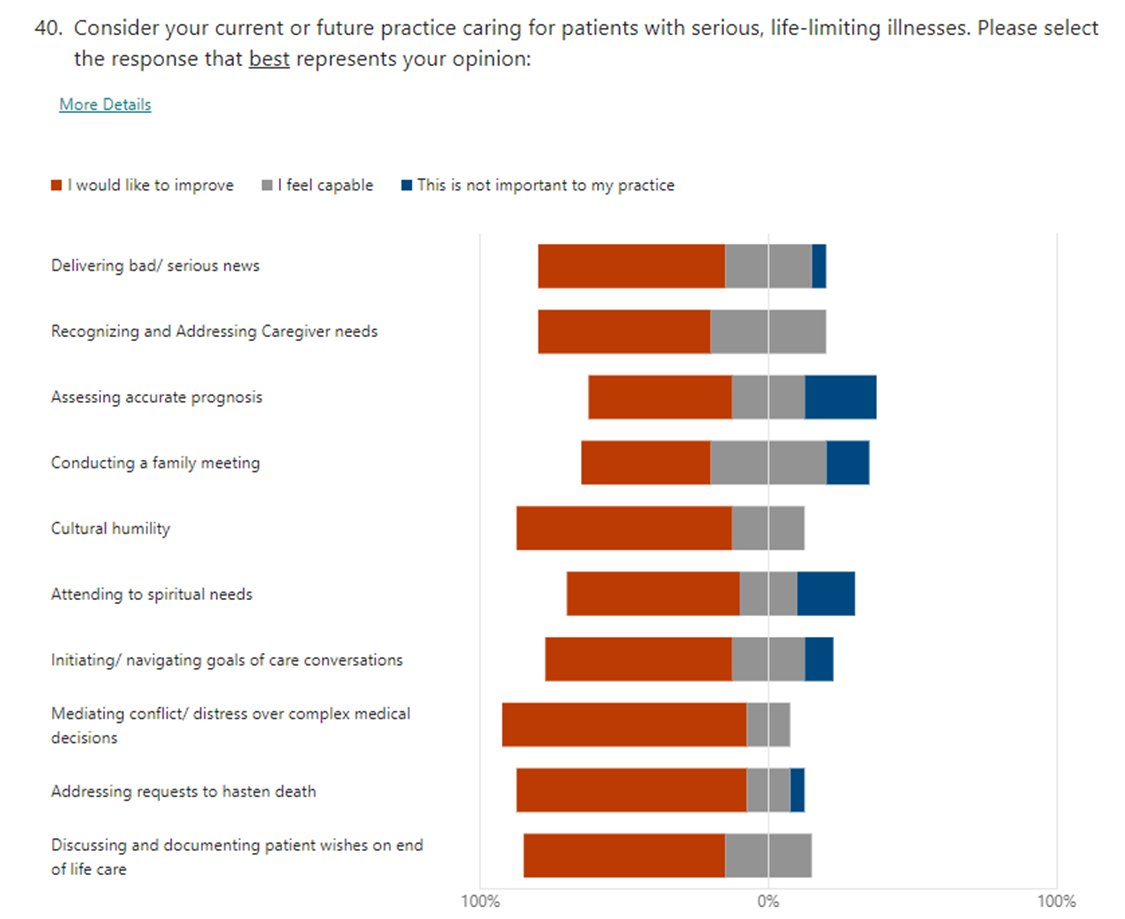
Figure 2. Palliative Scholars Learning Goals
Scholars were asked to articulate their personal Palliative Scholars Program goals (Figure 2). Out of a total of 59 goals, 46 (78%) goals were rated as “fully accomplished” and 12 (20%) additional goals as “accomplished.” Only 1 goal was rated “neutral”. Pre- and post-course evaluations demonstrated increased knowledge, with 100% indicating that they gained valuable communication skills to discuss advance care planning and goals of care (55% strongly agree; 45% agree). Participants also expressed increased comfort, perceived self-competence and efficacy in managing palliative care issues. Scholars reported empowerment and motivation to continue learning and be champions for Palliative care principles and competencies at their primarily rural settings of care.
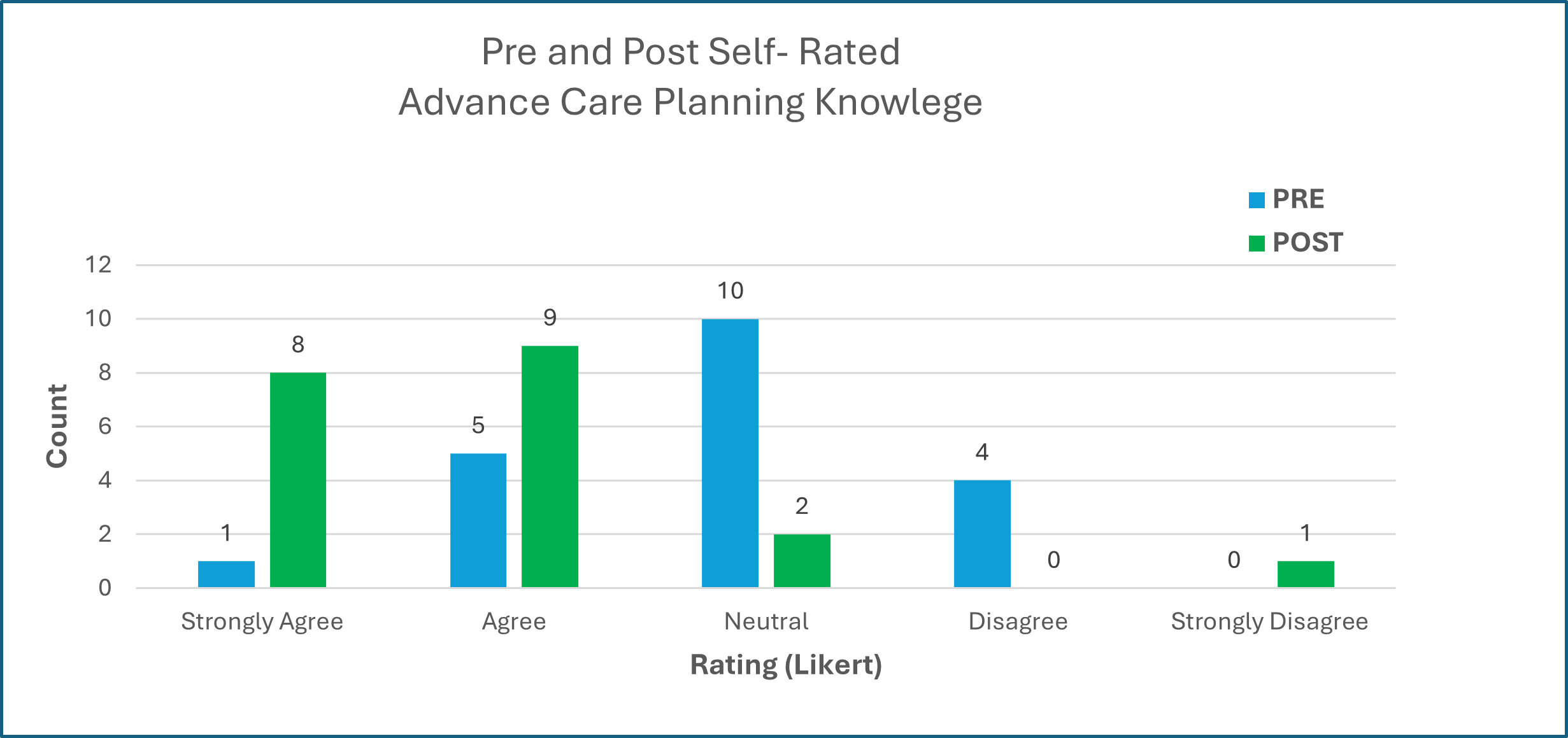
Figure 4. Advance Care Planning Knowledge: Prior to the practicum, 30% indicated having sufficient knowledge regarding Advance Care Planning versus 85% post-practicum.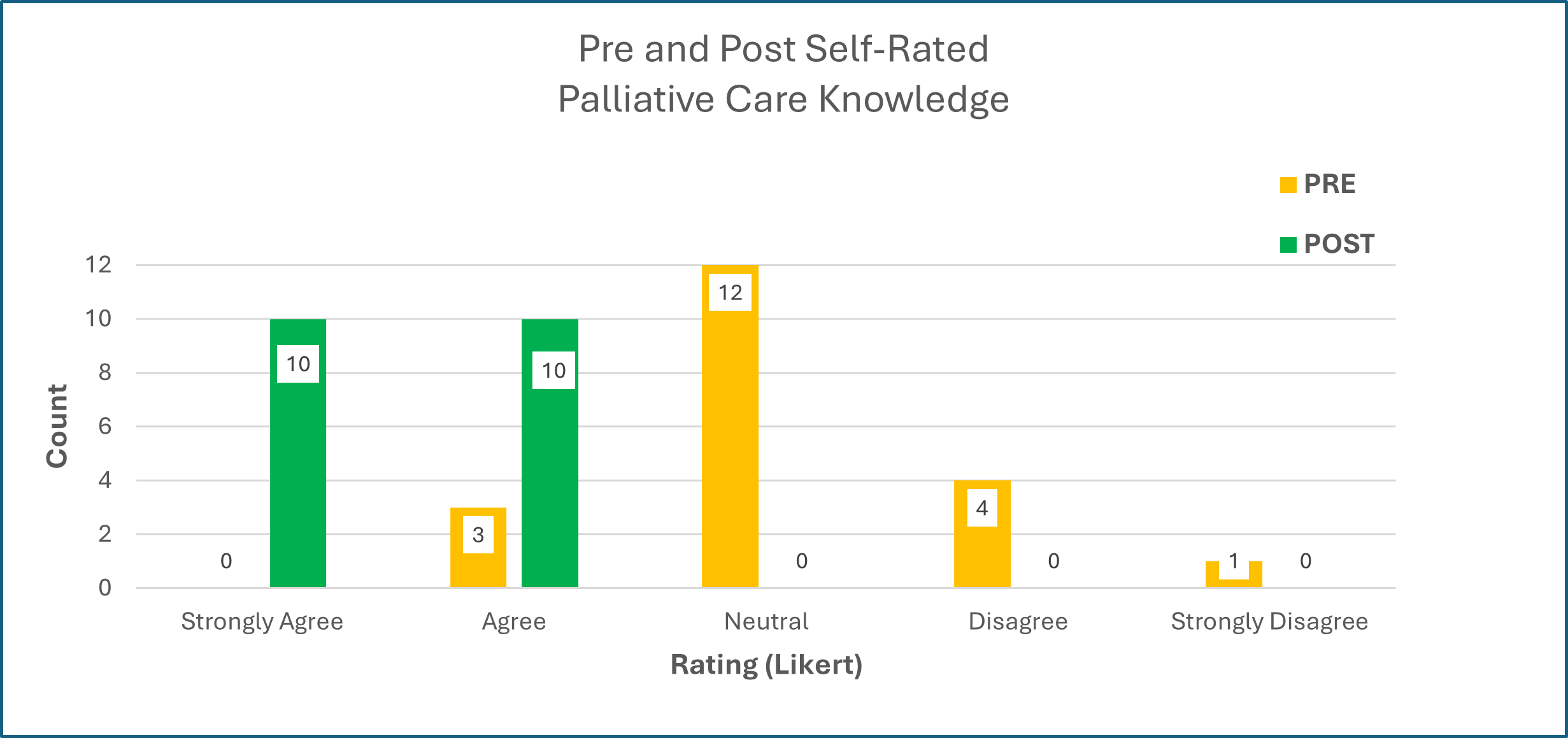
Figure 5. Palliative Care Knowledge: Prior to the practicum, 15 % indicated having sufficient knowledge regarding Palliative Care versus 100 % post-practicum.
Over 90% of the participants expressed high satisfaction with the program meeting their diverse needs for training that include discussion of prognostication, breaking bad news, pain, and symptom management, navigating team dynamics, and value-based discussions of goals of care. All the scholars indicated “Strongly Agree” regarding if they would recommend this Advanced Palliative Scholars practicum to others.
Subjective Feedback: Scholars provided feedback that they would like the training to contain even more content. Scholars also suggested that the program create additional, more advanced offerings in the future and expressed an intention to participate if available. Additionally, some scholars expressed a wish for TMS credit to help legitimize the training time with supervisors.
Conclusions: The Palliative Scholars model could provide one potential solution to the clear and present concern of workforce shortages of providers caring for those with serious illness. The model leverages the experiences of mid-career professionals from various disciplines and successfully utilizes multiple effective modalities of knowledge dissemination, expanding interdisciplinary role appreciation and teamwork, including immersive experiences grounded in adult learning theories. This highly personalized model integrates the individuals' goals with foundational palliative care principles and best practices and facilitates incorporation of best practices into their own site-specific workflows.
Contact: Sumathi.Misra@va.gov and Katharina.Echt@va.gov
Eastern Colorado GRECC Provides Better Service at a Lower Cost for Veterans Needing Help with Medication
BRAVe Home Meds (Boxed, Reconciled, Assistance at Veterans Home for Medications) is an innovative solution from the Eastern Colorado GRECC to avoid Community Care spending by insourcing medication management. Currently, the medical center spends millions of dollars on externally contracted home health RNs from community-based agencies to fill medication pill boxes. 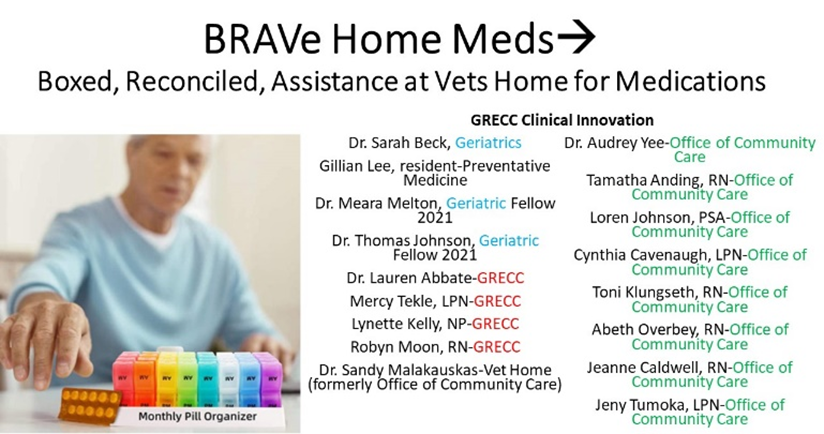
Working closely with front line staff from multiple services, GRECC clinicians identified inefficiencies and designed a comprehensive solution. BRAVe Home Meds utilizes existing VA infrastructure by deploying VA-employed LPNs to visit veterans' homes. These visits include medication management, health assessments, med box filling, and video consultations with geriatricians. By updating CPRS orders in real time, BRAVe ensures accurate and timely medication reconciliation while reducing administrative burden on primary care and the Office of Community Care (OCC), including fewer faxes and requests for signatures.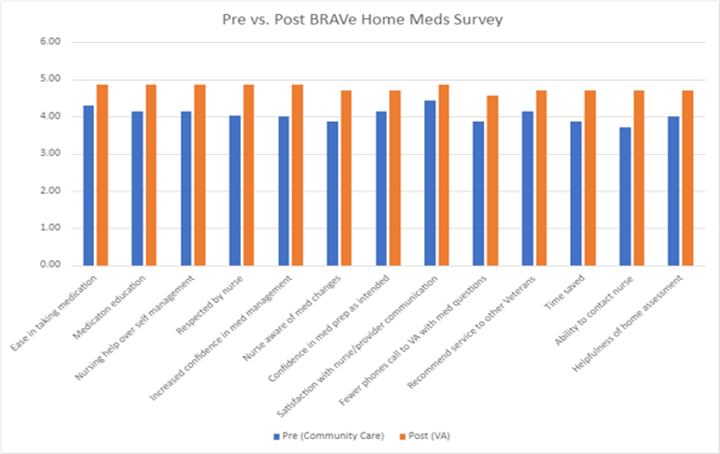
The program is more efficient and has comparable or better patient satisfaction than current practice at a significantly lower cost to the VA. The initiative spans multiple services lines (Geriatrics, GRECC, OCC) and demonstrates a commitment to delivering excellent care and utilizing resources efficiently for the benefit of older Veterans.
Contact: Kathryn.Nearing@va.gov
Care Partner Information Improvement Project (CPI-IP): creation of the Current Veteran Support Community Note to Facilitate Coordinated Care for the Whole Veteran
Background: Caregivers are key members of a Veteran’s healthcare team, who become increasingly important as a Veteran’s functional independence declines due to physical or cognitive changes. Despite the crucial role of caregivers, these individuals, and the specific roles they play in facilitating adherence to treatments and recommendations of healthcare professionals are not systematically identified. In prior clinical demonstration projects, The Minneapolis VA GRECC team faced barriers to efficiently and accurately identifying Veterans’ support community, including individuals identifying as caregivers. They found, as have others, that the lack of systematic documentation in the electronic health record (EHR) impedes quality improvement interventions with Veterans-caregiver dyads. To address this, the convened an interdisciplinary team to develop a documentation solution, gain input from potential users, and develop an initial roll out plan. This team included Allison Gustavson, DPT, PhD; Carla Amundson, MA; Hannele Nicholson, PhD, CCC-SLP, Huai Cheng, MD, MPH, MS, Erin Russell, BSN; Rebecca Brown, PhD, MEd, RN; Sarah Garrett, RN, MSN; Hilary Mosher, MD, MFA.
Approach: The Care Partner Information Improvement Project (CPI-IP) team convened as an interdisciplinary collaboration including nurses, a physical therapist, speech and hearing pathologist, and physicians, all with research, education, and clinical roles. Project funding was through GEC Clinical Demonstration funds. To contextualize the understanding of the problem and gain awareness of any upcoming or anticipated solutions, team members interviewed leaders in the Caregiver Support Program, queried a leader in the EHR modernization effort, and connected with researchers and implementation practitioners involved in caregiver research. They then began an iterative process of selecting a note title and template and subsequently incorporating feedback based on key informant interviews with VA staff from diverse disciplines and settings. In partnership with VA Informatics and Clinical Applications, including Michelle Millam, DNP, RN, NI-BC, Chief Nursing Informatics Officer (CNIO), Minneapolis VA, they produced a note for pilot testing and planned initial implementation informed by key informant responses.
Solution/Results: While improvement to the process of documenting and retrieving caregiver information was deemed important by healthcare professionals, there was a lack of consensus about who was primarily responsible for this task and what information should be included. Healthcare professionals may obtain, record, and use this information in diverse ways. The ability to update changing care needs and have current contact information were considered important for clinical decision making. We selected a note title, Current Veteran Support Community, to avoid confusion with Caregiver Support Program documentation and place the note early in alphabetical listing of note titles. The team included both free text and structured elements and allowed for more than one care partner to be listed, with free text options for detailing the types of assistance provided.
Lessons learned/anticipated challenges: The Current Veteran Support Community note seeks to create a shared area in which crucial “soft” data about care needs and social support, and contact data for support team members, can be documented and retrieved by any or all members of the healthcare team. A challenge to achieving timely, relevant, and useful documentation is that discussion of these issues can be complex, and their entry into the EHR can be conceptualized as both everybody’s job and nobody’s job. In other words, identifying, characterizing, and documenting these sorts of social data do not fit obviously into an assigned workflow. Rather, a full picture of a Veteran’s care community is collaboratively assembled and evolves unpredictably through time. This realization has influenced the planned implementation approach, in which they will test the perceived utility of this note by alerting clinical champions that it is available, rather than requiring or assigning completion. The team plans to track adoption and recorded content during stepped implementation efforts.
Implications: EHR features can both facilitate and impede the work of documenting and retrieving information about an individual Veteran’s support community. Effective interprofessional collaboration and coordination can be strengthened by making asynchronous communication about social supports easily available in the EHR. As they move into implementation of the note, the CPI-IP team anticipates learning more about how the distributed work of documenting crucial social information can be effectively supported in the EHR and related workflows. The experience underscores the value of agile, flexible, and local innovation within the EHR to facilitate quality improvement efforts.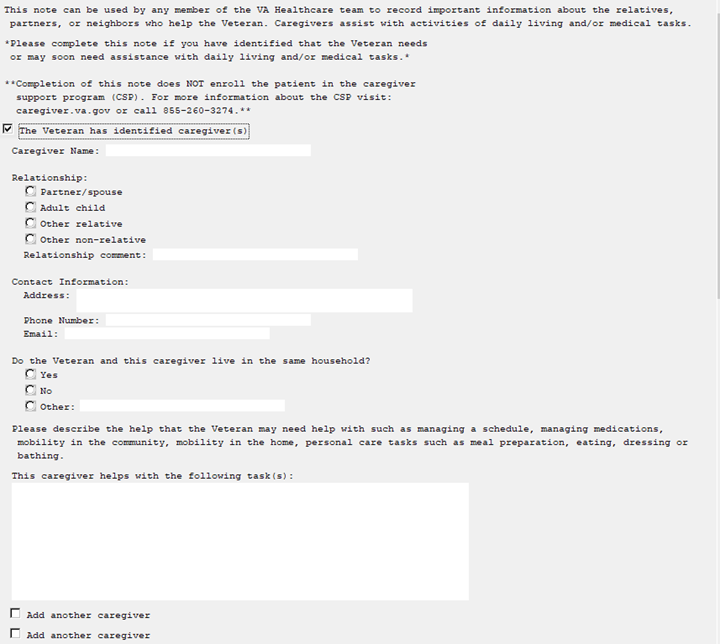
Contact: Allison.Gustavson@va.gov
KEEPING CURRENT
National Coordinating Center for VA Advanced Fellowship in Geriatrics to Host Event at Gerontological Society of America Annual Scientific Meeting.

The National Coordinating Center for the VA’s Advanced Fellowship in Geriatrics invites our VA and GRECC colleagues to join us for two events at the annual scientific meeting of the Gerontological Society of America (GSA) in November. We’d love to see you there!
Contact: Colleen.Hursh@va.gov
Dr. Makaroun attends White House Gun Violence Prevention Event
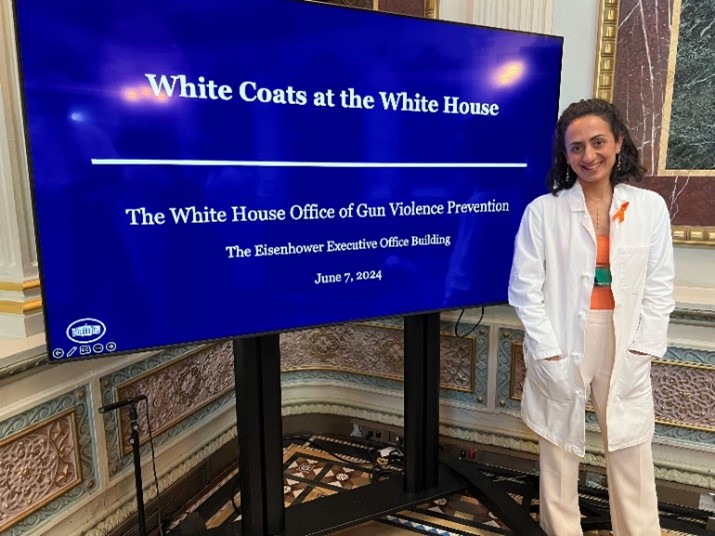 Lena Makaroun, MD, MS from the VA Pittsburgh Healthcare System Center for Health Equity Research and Promotion (CHERP) and the Technology Enhancing Cognition and Health (TECH-GRECC) was invited to attend the White House Gun Violence Prevention Event on June 7th, 2024 as a representative of the American Geriatrics Society (AGS) in recognition of her involvement in the American College of Surgeons’ Healthcare Coalition for Firearm Injury Prevention and her HSR-funded research on elder mistreatment and violence in older adults.
Lena Makaroun, MD, MS from the VA Pittsburgh Healthcare System Center for Health Equity Research and Promotion (CHERP) and the Technology Enhancing Cognition and Health (TECH-GRECC) was invited to attend the White House Gun Violence Prevention Event on June 7th, 2024 as a representative of the American Geriatrics Society (AGS) in recognition of her involvement in the American College of Surgeons’ Healthcare Coalition for Firearm Injury Prevention and her HSR-funded research on elder mistreatment and violence in older adults.
Dr. Makaroun is an HSR Career Development Awardee whose research examines health-related social risk factors for older adults, with a specific focus on elder abuse. Her current VA HSR-funded work aims to improve detection and response for elder abuse among older Veterans in VHA. The event brought together numerous healthcare professionals who treat and educate patients impacted by firearm violence. Speakers included Gregory Jackson Jr. and Rob Wilcox, Deputy Directors for the White House Office of Gun Violence Prevention.
Dr. Makaroun used the opportunity to advocate for the important impacts of gun violence on older adults, including the high rate of firearm suicide in this population and the need for greater attention to addressing firearm safety in those with cognitive impairment and dementia.
Staff News
Awards

Dr. Dittus Honored with Career Achievement Award
Dr. Robert Dittus, GRECC Director and Director of the Quality Scholars Fellowship Training Program at the Tennessee Valley VA, was recently recognized with the 2024 Worthen Awards Career Achievement Award. In the past 40 years, Dr. Dittus has created innovative programs to enhance training in research and quality improvement for VA trainees. Among his accomplishments, he served as the founding director of the Nashville VA Quality Scholars program and has mentored countless individuals, including 137 interprofessional fellows and junior faculty, 71 quality scholars.
 Dr. Pulia Elected as Fellow of American Speech-Language-Hearing Association
Dr. Pulia Elected as Fellow of American Speech-Language-Hearing Association
Dr. Nicole Rogus-Pulia of the Madison VA GRECC has been elected as a fellow of the American Speech-Language-Hearing Association (ASHA) in recognition of her accomplishments in the field of dysphagia. In her VA role, she serves as Director of the national VA multi-site Intensive Dysphagia Treatment (IDT) Program and Associate Director for Research Training and Career Development for the Advanced Women’s Health Fellowship. She will be honored at an awards ceremony at the ASHA national meeting in December 2024.
SUBMIT TO FORUM ON AGING
We welcome submissions from GRECCs for this news magazine, including:
- Updates and results about research, education, and evaluation efforts and clinical innovations
- Notices of awards, grants, training opportunities
- Staff news
- Photos or images to accompany your submission
GRECC Forum on Aging is published by the VA William S. Middleton Memorial Veterans Hospital and Clinics – Madison Geriatrics Research, Education, and Clinical Center.
Elizabeth Chapman, MD, Editor
For inquiries, please contact:
Madison VA GRECC
2500 Overlook Terrace
Madison, WI 53705
Phone: 608-280-7000
Fax: 608-280-7291
To provide feedback about Forum on Aging, please contact: Elizabeth.Chapman3@va.gov
Sponsored by the Office of Geriatrics and Extended Care, VACO