More Than Medicine

Veterans at the Truman Veterans Hospital in Columbia, MO participate in a health coaching session as a part of facility's the Integrative Health and Wellness Coaching program.
The following story was originally published in the Columbia Missourian and has been re-published here with permission from the editor.
MORE THAN MEDICINE: Veterans' Hospital takes wellness approach to combat Veteran health problems
Opioid addiction, heart disease and post-traumatic stress disorder are some of the most common health issues among Veterans, and Truman Veterans' Hospital is increasingly finding that the path to recovery for Veterans is through wellness. The Veteran's hospital has been doing wellness for five years. But last year, it brought together the pieces, formalized its efforts and named it the Integrative Health and Wellness Program.
The focus is on Veterans' health as a whole. This year, the Veterans hospital brought on three new health coaches as part of the program for a grand total of four full-time staff — soon to be five. "Our biggest challenge is changing a 100-year-old system," said Jeremy Jobe, one of the new health coaches at the Veterans hospital.
That system's central focus has long been prescribing medications. But that doesn't take in the big picture — the mental, physical and spiritual health of the Veteran. "The pharmaceutical route only takes care of 20 percent of the problem," Jobe said. The other 80 percent of getting healthy is up to the person. "You're your best advocate... medication... everything," he said.
It's not just about educating Veterans about "whole health," Jobe said. It's also an opportunity for physicians to see the benefits of wellness. In the end, what the health coaches hope the program looks like is this: A veteran goes to see a physician who refers him or her to the program. The Veteran goes to coaching sessions and then returns to the physician with a personalized health plan.
The plan gives the physician a sense of the Veteran's health priorities when creating a plan of care. Together, coaches and physicians can change the outcome for Veterans by sharing the responsibility for the patient's outcome, Jobe said.
Opioids, be gone
That same Veteran-centered approach is in use in the Integrative Health and Wellness Program, formerly the Whole Health Program, said April Leverett, manager of the program. She describes herself as a longtime advocate of non-traditional approaches to Veterans' health. Asking questions like, "What really matters to you in your life?" "What brings you a sense of joy and happiness?" "What is your vision of your best possible health?" effectively shifts the focus to the Veteran, she said. "We empower and equip Veterans to live the life that they want to live," Leverett said, "not the one we think they are supposed to live."
Between 2010 and 2015, opioid addiction rose 55 percent among Veterans. They're also twice as likely as non-veterans to accidentally overdose, according to a report from the Center for Ethics and the Rule of Law. Leverett said she thinks the program is one of many initiatives that have impacted reduction in opioid use.
Veterans can participate in Integrative Health and Wellness Coaching. This approach involves face-to-face or over-the-phone consultations with coaches, and the hospital plans to add a virtual option sometime soon. It uses mindfulness to treat mental or physical problems, including addiction, by pushing Veterans to be mindful of their purpose and life aspirations when making choices.
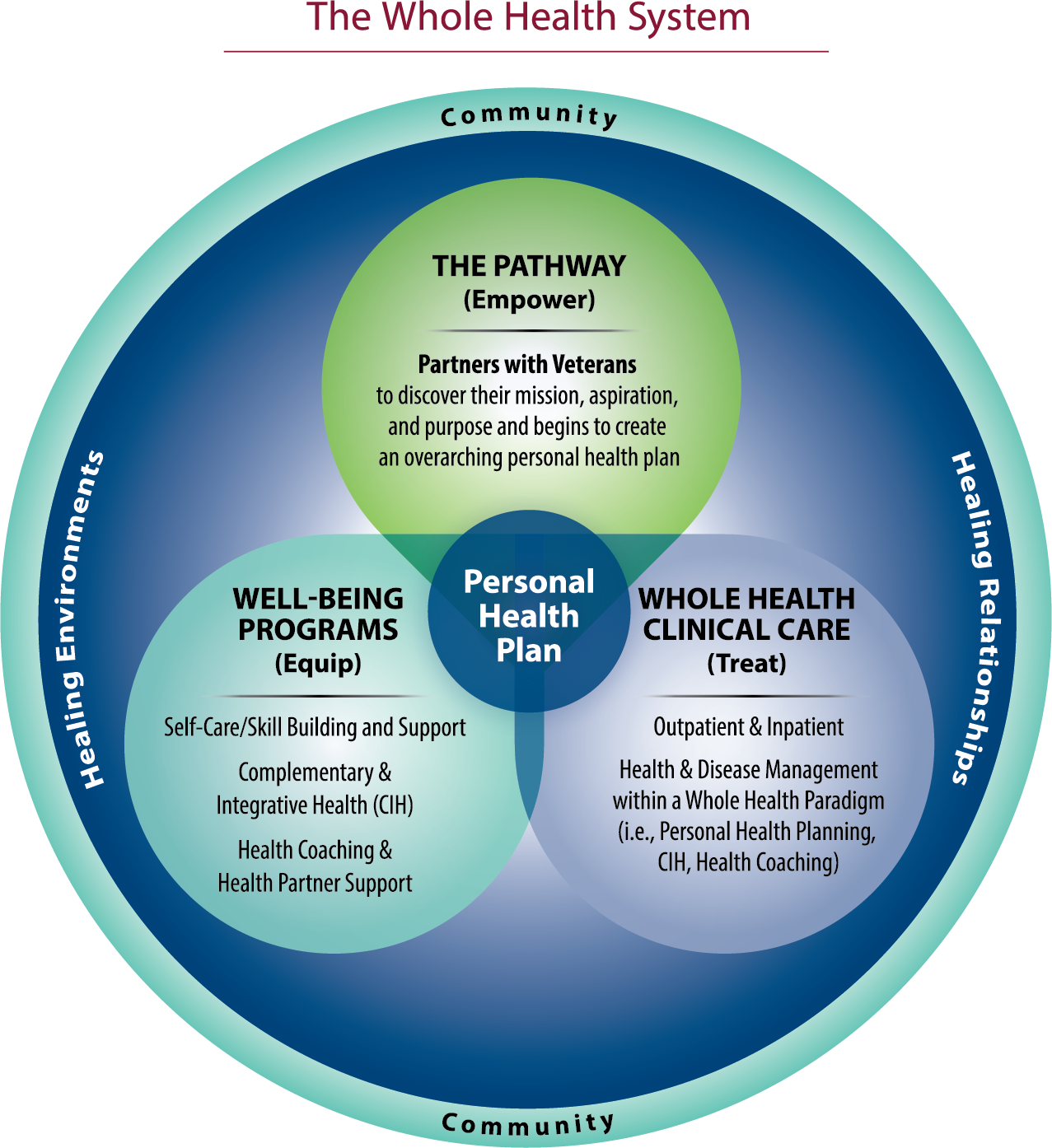
Diagram of the Whole Health System 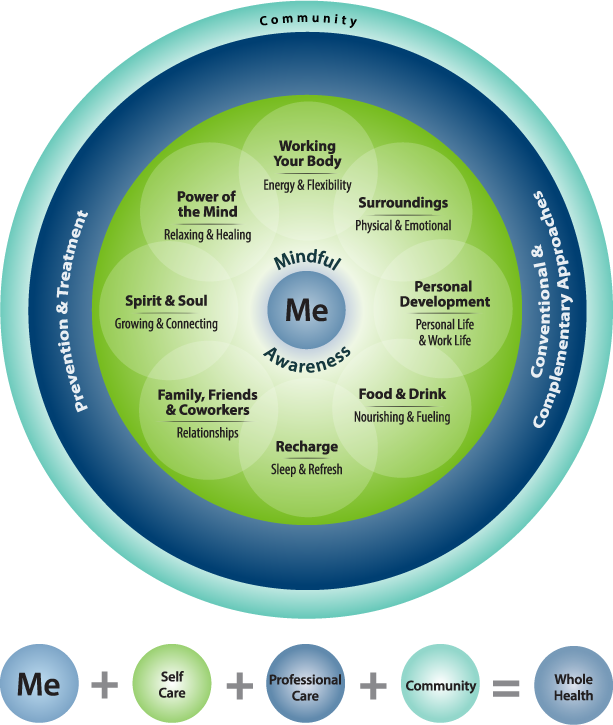
Diagrams of Personalized, Proactive Health and Well-being Model
Veterans rate themselves on where they think they are in each of the areas and choose which area or plan they want to start with.
"Tell me what matters to you," is the prompt that changes the conversation with Veterans from advising to listening, said Jobe, who is a Veteran himself. It focuses on what the Veteran thinks he or she needs, not what anyone else thinks the person needs. The plans can include making dietary changes and taking classes like tai chi, yoga and guided meditation that are offered under the Integrative Medicine program, a branch of the Integrative Health and Wellness program.
"It’s their choice," coach Jessica Streit said.
Jobe said: "Your agenda is our agenda."
Into action
Elton Larry Dan Lamberson, 63, who served five and a half years in the military, was one of Jobe's patients in the Integrative Health and Wellness program. He started having trouble with his health and began falling. When he began physical therapy, his therapist asked if he would be interested in the program. Soon after, Lamberson began meeting with Jobe to devise a plan. Going into the program, Lamberson did not have a goal in mind. All he knew was that he needed help and answers.
"They let me make most of my own choices," Lamberson said. "They let me ask the questions, and they give me the answers." Lamberson said the program is non-judgmental and he has enjoyed it.
While going through the eight stages of health, he saw how each was connected. By focusing on mindfulness, Lamberson has learned how to be mindful while eating. For example, Lamberson and others in the program practice consciously eating by placing a piece of food in their mouth, letting it sit there without chewing, feeling the texture, tasting it and noticing if it melts.
He has also learned how to be mindful of the present moment. He talks about a cartoon titled "Mind Full, or Mindful?" that illustrates how to be present. In it, a human figure is walking a dog. A "thought bubble" shows the person thinking about everything except the immediate environment. Meanwhile, the dog is only focusing on what lies ahead, physically.
Elton Larry "Dan" Lamberson practices tai chi Wednesday at the Truman Veterans' Hospital in Columbia. When Lamberson started tai chi more than five months ago, he required a cane to walk but has spent the last four months without a cane. MARTA PAYNE
"I don't think you need to have an emotional problem at all to go through (the program) and gain something," Lamberson said. "Most of the people coming here have a medical problem, but not all of them have an emotional problem." He has become a big booster of the Integrative Health and Wellness Program. Although Lamberson no longer uses the coaching part of the program, he still attends group sessions like tai chi.
As a result, he said, he has become more aware of his "numbers" — his weight, blood pressure, etc. — and is happier overall. "It made a world difference in my life," he said. "You make better decisions and change (mentally)."
Heart health, inside and out
Mindfulness is also being applied to treatment of Veterans with heart conditions. They're at a much higher risk for heart disease than the general public, said Dr. Anand Chockalingam during a Heartful Living workshop recently held at the veterans hospital. Chockalingam, an associate professor of clinical medicine in the cardiovascular division at MU, gave an 8-week workshop at the Veterans hospital about how meditation can lead to a healthy lifestyle.
By engaging the body in heartful living, Chockalingam said, the health improvements come naturally. "We are the most powerful nation, but we have the most health issues," he said. Mediation can change this, he said.
Meditation is not only about taking time to clear the mind. It also involves a new outlook on life. Instead of focusing on the good and bad foods, it teaches people to feel hunger and celebrate the presence of friends, family and food, he said. When it comes to a diet and exercise, Chockalingam recommends a plant-based diet with cardio three days a week. He emphasizes doing whatever exercises a person loves that are both challenging and require skill.
Leslie Barnes leads a group of six people in tai chi during a class Wednesday at the Truman Veterans' Hospital in Columbia. Before she stated teaching tai chi six years ago, Barnes worked for 23 years as an operating room nurse at the veterans hospital. MARTA PAYNE
The heart needs a healthy diet, exercise and state of mind to function optimally, he pointed out.
He uses the acronym HEART:
- Humility
- Empathy
- Aspirations
- Reciprocation
- Trust
"Heartfulness is the total, intense and complete devotion needed to succeed," Chockalingam said.
TLC for PTSD
Dr. Grant O’Neal, a psychologist who works with the Post-traumatic Stress Disorder Clinical Team at the Veterans hospital, acknowledges the benefits of the Integrative Health and Wellness program and refers patients to it as needed. However, he takes a different approach to the whole health of his patients. "I often review a 'Therapeutic Lifestyle Changes' (TLC) list of eight approaches to well-being," O’Neal said. The eight approaches to well-being are:
- Relationships
- Giving back
- Exercise
- Nutrition
- Relaxation
- Recreation
- Nature
- Spirituality
There are similarities between wellness and TLC like exercise, nutrition, relaxation and spirituality. By not focusing solely on exercise and nutrition, Veterans hospital specialists have encouraged veterans to embrace a different type of mindset in order to live life to the fullest.
The program is available to all who are eligible for Veterans Affairs health care, and all are encouraged to join. Leverett said: "The VA is in a unique position to show the country how this can work."





















