Personal Development
Personal Development is one of the areas of self-care in the Circle of Health and involves all the things a person can do to grow in some fashion. Examples of personal development topics that can be incorporated into Whole Health Personal Health Plans (PHPs) include building hope and optimism, finding balance in life, trying new creative pursuits and skills, volunteering, practicing gratitude, building social capital, lifelong learning, improving financial health, and building humor. Cultivating resilience is fundamentally important to personal development as well. This overview builds on the material featured in Chapter 7 of the Passport to Whole Health.
Key Points
- Personal development has many facets. Work with Veterans to decide which one they would like to focus on first. Be sure to tie their choices in with their values and what really matters to them (their Mission/Aspiration/Purpose).
- The various aspects of personal development are beneficial to health. For example, quality of work life contributes to better health, as does volunteering. Resilience counteracts burnout and is protective in many other ways. People who are more hopeful and optimistic live longer. Employment and financial health are important determinants of well-being too.
- This overview discusses 16 potential personal development topics. Keep asking yourself about how each of them could be incorporated into a PHP, when appropriate.
Meet the Veteran

Sarah is a 42-year-old Navy Veteran who now works in health care as a certified nursing assistant (CNA). She comes in to see her primary care clinician for her yearly exam. She is divorced and has a 14-year-old son and a 12-year-old daughter at home.
Sarah reports some fatigue and difficulty sleeping. Her main sources of stress are managing her household, raising her children as a single mother, working part-time at a local hospital, and never seeming to have enough time or money to accomplish her goals. She receives minimal child support from her ex-husband, who is only marginally involved in the children’s lives. She does have a few good friends, and her parents live nearby and help her with the children. She is struggling with work-life balance and finding time for herself.
She currently experiences distress and anger about her ex-husband’s and his family’s lack of involvement with and support for their children. She worries about having enough money to provide for her family, to the point where the worries interfere with her ability to enjoy her time with them. Financial health is a concern, because she tends to overspend when she is stressed and has high balances on her credit card that she wants to pay down.
Sarah was asked to complete a Personal Health Inventory (PHI) prior to her next visit. As she worked through the PHI, it became apparent that she had few ways to manage stressors besides shopping and social support from friends and family. She notes that she needs to make her own well-being a higher priority and develop additional strategies for finding balance in her life. In the past, she used to have hobbies, such as creative scrapbooking and drawing, and she misses doing these activities. She rarely has time to exercise and reports she gets most of her movement at work on the hospital floor.
Introduction
Personal development is a broad term. It encompasses many activities:
- Improving awareness and identity
- Developing talents and potential
- Building social capital
- Nurturing positive emotions
- Fostering lifelong learning
- Enhancing creativity
- Improving quality of life
- Contributing to the realization of dreams and aspirations
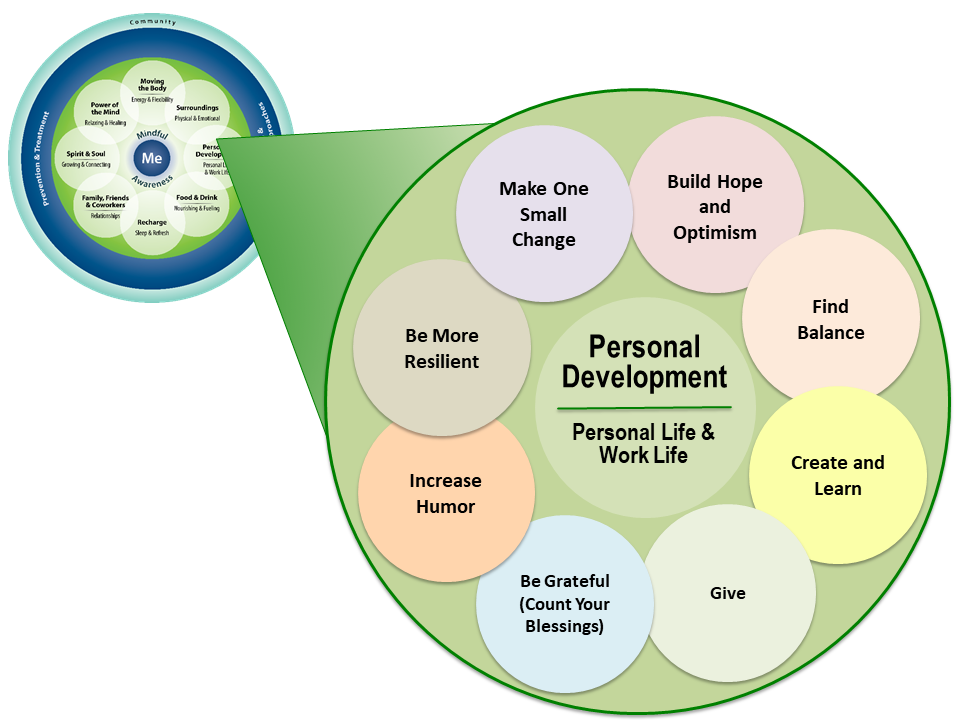
In Fiscal Year 2017, Whole Health skill-building courses were created to help Veterans focus in on specific “subtopics” related to each area of self-care. Figure 1 shows the subtopic circles for Personal Development.
Carl Jung and Abraham Maslow were early contributors to personal development as an aspect of health:
- Carl G. Jung (1875–1961) made contributions to personal development with his concept of individuation.[1] He defined this as the drive of the individual to achieve the wholeness and balance of the Self, which he considered the central process of human development.
Abraham Maslow (1908–1970) developed the well-known “hierarchy of needs.” This model suggests that psychological health is based on meeting basic human needs that have different levels of priority (refer to Figure 2).[2] Only when basic needs are met do we have the energy and opportunity to fully engage in higher levels of personal development. Maslow referred to these higher levels as “self-actualization.”[3]

-
Both Jung and Maslow believed that individuals have a strong need to realize their full potential.
In business or organizational settings today, personal development can be seen as an investment, with the end result being an increase in the economic value of employees. The goal of investing time and money into the personal development of employees might be to increase creativity, innovation, quality and/or productivity.,
More recently, the field of positive psychology has emerged with contributions to personal development. Positive psychology has been defined as those, “conditions and processes that contribute to the flourishing or optimal functioning of people, groups and institutions.”[4] It is concerned with positive human experiences. These include, but are not limited to
- Gratitude
- Hope and optimism
- Values and meaning
- Forgiveness
- Positive relationships
Research in the area of positive psychology has been steadily building, and it is clear that focusing on positive experiences can be a powerful way to help individuals and groups be successful. [5]
This module will focus on a number of ways to foster personal development. Become familiar with them, and add others to the list of possibilities as you see fit. Some of the key research in these areas will be highlighted. In many instances, the content pertains specifically to clinicians, but much of this material is applicable to everyone. For additional information related to “Care for the Caregiver,” refer to the module, “Implementing Whole Health in Your Own Life: Clinician Self-Care.” The following topics, chosen in part because they have been researched to some degree, are covered in this overview:

Mindful Awareness Moment
Choosing an Area of Personal Development
Listed above are the 16 areas of personal development discussed in this overview. Take a few moments to choose the one or two that you are most inclined to work on yourself.
- What led you to make your choice(s)?
- How might you focus more on that area? Outline two or three specific actions you can take to make progress in this area.
- In what ways will that area of personal development enhance your overall health?
Quality of Work Life
Most people spend a third of their adult lives working. Quality of work life (QWL) has a substantial influence on health and well-being. QWL relates to a person’s feelings about all the dimensions of their work, ranging from salary and benefits to job security, workplace safety, relationships at work, and how work contributes (or does not) to a person’s sense or meaning and being valued. Job dissatisfaction, workplace injuries, stress, discrimination, and many other aspects of working life can have a profound effect on health. QWL is important for people whether or not they are paid for it and whether or not it is done inside or outside of the home.
A great deal of what is known about QWL comes from studies of health care providers. Health care environments, like many work environments where QWL tends to be low, are known to be demanding, both physically and psychologically.[6] Nurses are one group of professionals whose QWL has been examined quite closely. Nurses’ QWL is linked to:
- Patient outcomes[7,8]
- Staffing levels[9,10]
- Staffing mix[11]
- Work schedules (and number of hours nurses worked)[12]
- Overtime requirements[10]
Knox and Irving (1997), in a meta-analysis of QWL among nursing staff, found that the following characteristics of the workplace positively influence QWL[13]:
- Autonomy
- Lower levels of work stress
- Favorable relations with supervisors
- Appropriate job performance feedback
- Opportunities for advancement
- Low levels of role conflict
- Fair and equitable pay levels
These findings are likely to be relevant when it comes to QWL for other professions. A large 2017 review of 37 studies found, for workers in general, that “high job demands, low job control, high effort-reward imbalance, low relational justice, low procedural justice, role stress, bullying and low social support in the workplace are associated with a greater risk of developing common mental health problems.”[182]
In considering the relationship between health and QWL, keep the following in mind:
- High levels of job stress lead to more days out of work and a greater need for activity limitations.[183]
- Shiftwork has a negative effect on health. Recent studies have highlighted that, for the nearly 25% of people who do shift work, there are significant negative effects on sleep, substance use, cognitive function, mood (anxiety and depression), quality of life, and workplace safety.[184]
- QWL is closely linked to burnout. Burnout typically comprises feelings of cynicism/depersonalization, loss of enthusiasm for work, and a low sense of personal accomplishment.[185] Burnout (according to data for physicians and other people working in helping professions), is tied to excessive workload, clerical burdens, work-home challenges, lack of input or control around issues that affect work experience, leadership culture, and the organizational support that is or is not present in a workplace.[186] Physician burnout rates, as an important example, have ranged from 38-63% in various studies over the past 11 years.[14,187] Rates vary, but burnout also occurs at high rates for people in other “helping” professions, including for social workers, pharmacists, and mental health professionals. Teachers, lawyers, mental health professionals, and many other groups demonstrate high rates of burnout. So do police officers, first responders, clergy, and teachers.[188] Anyone can potentially experience burnout in the workplace.[189]
- Unemployment itself has negative effects on health, including contributing to anxiety and depression, diabetes, and cardiovascular disease.[190,191]
Balance between work, family, and other obligations can also have a profound impact. This is discussed later in this review, in a separate section.
Resilience
Building resilience is a fundamental goal of personal development. Resilience, although multifaceted, is commonly defined as involving a positive adaptation to adversity.[15] Resilience includes being able to[16]
- Adapt to changing environments
- Identify opportunities
- Adapt to constraints
- Bounce back from misfortune and challenges
The generation of positive emotions has been associated with resilience.
- Positive emotions broaden our thinking/behavior repertoires, helping us adapt in the face of change or disruption.[17,18]
- Individuals high in resilience do not actually lack negative emotions. Their levels of negative emotions are comparable to those of less-resilient peers. What occurs, however, is that they generate more positive emotions. These researchers conclude that resilience generates positive emotions and positive emotions and resilience build on each other. [16]
Exploring resilience in physicians, Zwack and Schweitzer conducted over 200 semi-structured interviews investigating prototypical processes and key components of resilience-fostering preventive activities.[19] The following themes emerged as being helpful for promoting resilience for physicians (they are relevant for nonphysicians as well):
- Gratification from the doctor-patient relationship, including the following:
- Showing interest in the patient as a person seemed protective in the presence of monotony (Again, this highlights the importance of the personalized and patient-driven approach)
- Feeling that their opinion matters
- Experiencing patient appreciation and gratitude
- Appreciating the medical efficacy of the intervention
- Resilience Practices:
- Engaging in leisure time activity to reduce stress, especially:
- Sports and physical activity
- Cultural activities such as music, literature, art
- Quest for and cultivation of contact with colleagues
- Cultivation of relationships with family and friends. See the “Family, Friends, & Co-Workers” module of the Whole Health website
- Proactive consideration of the limits of one’s skills, handling complications, and addressing treatment errors
- Personal reflection—consciously and regularly taking time to reflect; for approaches to facilitate this, refer to the “Mindful Awareness” overview
- Self-demarcation—physician ability to maintain clearly defined boundaries
- Cultivation of professionalism including continued learning and education
- Self-organization—individual routines and time structures, delegation, and setting priorities all play a role
- Ritualized time out that can occur on a daily, weekly, and/or annual basis
- Spiritual practices—refer to the “Spirit & Soul” module on the Whole Health website
- Other interventions: resilience workshops, cognitive behavioral interventions, small-group problem-solving and sharing, [20]which can be combined with reflection, mentoring, mindful awareness, and relaxation techniques
One concept that is closely linked to resilience, particularly for Veterans, is Post Traumatic Growth (PTG). First discussed in the mid-1990’s, PTG has been defined as “positive psychological changes experienced as a result of the struggle with trauma or highly challenging situations.”[192] PTG is not an alternative to negative consequences of trauma but is best thought of as running parallel to them. It can be associated with several positive changes (or “evolutionary possibilities”) related to:[193]
- Philosophy of life
- Relationships
- Self-perception and identity
- Self-confidence
- Capacity to handle difficulties
- Flexibility
- Greater openness to others
- Discovering new possibilities
- Greater appreciation of life in general
Cognitive Behavioral Conjoint Therapy is one therapeutic approach that specifically includes PTG. There are now well over 4,000 studies related to PTG in the medical literature.
Happiness
At least since the time of Aristotle, philosophers and religious leaders have asked the question, “How can we become lastingly happier?”[21] The field of positive psychology has researched this topic in the last decade and highlighted a variety of practices to foster the conditions of happiness. A 2023 systematic review that surveyed determinants of happiness from a global perspective concluded that happiness includes multiple determinants, classed under three main categories: 1) Health, 2) Hope and 3) Harmony.[194]
Happiness is an especially important aspect of personal development for health care clinicians to cultivate. When happiness and career satisfaction decline for health professionals, it negatively impacts the work that they do. For example, studies have shown that physicians who report low levels of happiness are more likely to change jobs, have less satisfaction with patient encounters, provide lower-quality patient care, and negatively influence office morale.[22-25] Happiness can be improved and increased when clinicians shift focus to building skills to manage or limit the workload, improve feelings of work accomplishment, improve career satisfaction and meaning, and manage distress related to patient care.[26]
A widely used theory of happiness includes three distinct aspects[26,28]:
- Positive emotion and pleasure (the pleasant life). This includes positive emotions about the present, past, and future and learning skills to increase the intensity and duration of these emotions.
- Engagement (the engaged life). The focus here is pursuing engagement, involvement, and absorption in work, as well as with intimate relations and leisure. An individual’s highest talents and strengths (“signature strengths”)[29] are identified and used.
- Meaning (the meaningful life). Pursuit of meaning is also central. It involves using signature strengths and talents to belong to and serve something that one believes is bigger than oneself.
Additional happiness research supports the following key findings:
- The most satisfied people are those who orient their pursuit in life toward all three of the above aspects of happiness, with the greatest weight carried by engagement and meaning.[30]
- Happiness is causal and brings more benefits than just “feeling good.” Happy people are found to be healthier, more socially engaged, and more successful. These things all beget even more happiness.[31]
- Seligman tested a signature strengths exercise to increase happiness.[21] After identifying their personal strengths, participants were asked to use them in daily life over a one-week period. They found that this exercise significantly lowered depressive symptoms. Positive effects lasted at least six months.
- Research suggests that there are very concrete benefits to increased happiness. Both prospective and longitudinal studies show that it precedes and predicts positive outcomes such as better life outcomes, financial success, supportive relationships, mental health, effective coping, physical health, and longevity.[16] A large 2024 review concluded that happiness may be “directly associated with improved health parameters and reductions in debilitating symptoms.”[195] Happiness has been linked to decreased risks of hypertension.[196]
Family support was strongly related to concurrent happiness.[32]
Hope and Optimism
Charles R. Snyder, PhD, a pioneer in hope research, developed the definition of hope used in mental health research. His model of hope has three major components:
- Goals related to a certain situation
- Agency, the belief in one’s personal ability to make things happen to reach the goals
- Pathways, the methods and plans that allow individuals to achieve goals in any situation
Optimism versus hope
Optimism appears to be different from hope, even though the two are related.
- Optimism is more general. It involves the thought/sense that good things will happen in the future.
- Hope, unlike optimism, is more activating in that it helps someone move toward what he or she wants to happen, given that it includes goals, agency, and pathways.
Benefits of hope
Hope has been found to have numerous health benefits.[197] In one study, pediatric clinicians with a higher trait of hope were able to enroll more children into a management program for asthma than clinicians with a lower trait of hope.[33] This suggests that the high-hopes clinicians were able to keep moving toward their goal, even though the situation had many obstacles and barriers. Hope has been linked to favorable outcomes for cancer patients and may be influenced not only by personality characteristics and the environment, but also by a person’s physiology.[197] It is important to palliative care patients, and has a potential benefit for people with chronic pain and other chronic illnesses.[198,199]
Clinicians themselves appear to benefit from hope. Hope can provide a greater sense that life is meaningful,[34] and it can also be a strong predictor of positive emotions.[35] Hope offers people a sense that life is meaningful and is linked to more positive emotions overall; it has significant potential benefit for helping people with mental health problems.[200,201]
Across settings, hope was also related positively to productivity. Lopez found that hope accounted for 14% of productivity in the workplace, which was greater than the influence of intelligence, optimism, or self-efficacy.[36]
Optimism and hope in chronic disease
Reviewers conducted a systematic review on hope and optimism and found that cardiac patients with higher levels of optimism had better outcomes in terms of physical health.[37] Results were not as clear with cancer patients, although it was noted that they suffered fewer negative changes in their condition. More subjective results occurred for the construct of hope although patients with higher levels had more satisfaction and a higher quality of life. A 2019 systematic review and meta-analysis found that optimism is associated with a lower risk of cardiovascular events and all-cause mortality. Certainly, more research needs to be completed, but we are beginning to understand the neuroscientific basis for hope and optimism, which will prove invaluable moving forward with therapeutic interventions.[202]
techniques for cultivating Optimism and hope
It is possible for people to learn to be more hopeful and optimistic.[203] For example, Hope Therapy exists as a specific protocol which has shown benefits for people in individual and group therapy settings.[204] Various mind-body skills training can be helpful in cultivating optimism, including imagery, self-forgiveness,, and meditation.[205-207] A 2019 study found that online mindfulness training can increase optimism as well.[208] We are beginning to understand some of the neurobiology of optimism, which may help us to cultivate it in ourselves and others even more effectively.[209]
Self-Compassion
We can often be so busy taking care of other people that we put our own self-care on the back burner. Without tending to our needs, we can be vulnerable to burnout and become less effective at work and in our personal lives. Research indicates that compassion for others is closely linked to self-compassion and ability to engage in self-care.[38-40] Thus, developing self-compassion may be pivotal (in health care professionals and others) for avoiding compassion fatigue, and it may enable a clinician to better manage being in close contact with the suffering of others.
Self-compassion involves directing care, kindness, and compassion toward oneself. Neff states that self-compassion involves “being open to and moved by one’s own suffering, experiencing feelings of caring and kindness toward oneself, taking an understanding, non-judgmental attitude toward one’s inadequacies and failures, and recognizing that one’s experience is part of the common human experience.”[41] Self-compassion has several features, including:[42,210]
- Self-kindness
When things go wrong, one treats oneself with kindness and care, and less directed criticism and anger. One is reassuring to oneself rather than critical. Self-talk is positive—encouraging and friendly.
- Common humanity
Recognizing one’s experiences, no matter how painful, are part of the common human experience. This reduces isolation and promotes adaptive coping.
- Mindful awareness
Mindful awareness helps foster a balanced perspective of one’s situation so that one is not carried away with emotion, being mindful of one’s feelings.
- Decreased negative behaviors/thought patterns
These include reduced self-judgment, isolation, and overidentification.
Benefits
Self-compassion is associated with higher levels of positive affect, optimism, and happiness,[43] lower levels of anxiety and depression,[44] and better functioning romantic relationships.[45] Self-compassion is associated with resilience to burnout and happiness and well-being in healthcare professionals.[46] Research indicates that self-compassion can act as a catalyst for health care professionals to provide compassionate care to others.[47-53] Self-compassionate people react to lab-based stressors in more balanced ways, with lower levels of negative affect and more realistic self-appraisals.[43,54] Self-compassion also predicts greater self-worth stability,[55] and a 2014 study found that having more compassion toward oneself paradoxically may make people more motivated to improve themselves.[56]
A 2011 meta-analysis found a large effect size when examining the link between self-compassion and depression, anxiety, and stress across 20 studies.[57] Self-compassion has been linked with experiencing better physical health through engagement in health promoting behaviors and lower levels of negative affect.[58,59] A 2020 systematic review found benefits for anxiety, depression, stress, and diabetes outcomes, such as A1c levels.[211] Self-compassion is associated with lower levels of subclinical cardiovascular disease as well.[212] Building self-compassion is helpful for weight management, and shows promise in the treatment of PTSD, autism, eating disorders, low back pain, and insomnia in addition to many other potential roles.[213-218]
Self-compassion has been found to be associated with numerous psychological strengths, such as happiness, optimism, wisdom, curiosity and exploration, personal initiative, and emotional intelligence.[43,60]
Increasing Self-Compassion
Self-compassion is a skill that can be learned and practiced. A 2019 meta-analysis of 27 trials found that various interventions increased self-compassion, and effect sizes were medium to large.[219] Short-term dynamic psychotherapy, compassion-focused therapy, the Mindful Self-Compassion course, and other offerings have been found to increase levels of self-compassion.[213]

Mindful Awareness Moment
A Brief Self-Compassion Practice
Compassion practices are one of many forms of mindful awareness practice. They are practiced in many spiritual traditions worldwide. These practices usually start with saying a few key phrases about yourself, before you move on to say them for others. These “others” may include a teacher, a loved one, someone you feel neutral about, a challenging person, a group of people, your co-workers, your patients, all of humanity, or even all living things. For now, just start with yourself.
Repeat the following phrases, out loud or to yourself:
- May I be safe and protected.
- May I be balanced and well in body and mind.
- May I be full of loving-kindness.
- May I truly be happy and free.
Repeat them again. Really focus on the meaning of each word.
Repeat them again. This time, focus on the phrase, and try to feel the intention of it. Many people focus on the heart area as they do so.
And repeat a fourth and final time.
How did you feel doing this? How do you feel now relative to before you started? Did you find it hard to say these phrases to yourself? Why or why not?
Forgiveness
Robert Enright, PhD, defined forgiveness as a “...freely made choice to give up revenge, resentment, or harsh judgments toward a person who caused a hurt and to strive to respond with generosity, compassion, and kindness toward that person.”[61]
There are a number of common denominators that arise in definitions of forgiveness[62]:
- Not forgiving involves ruminations that may be begrudging, vengeful, hostile, bitter, resentful, angry, fearful of future harm, and depressive.
- Forgiveness is a process rather than an event.
- Forgiveness of strangers or people with whom one does not want nor expect continuing contact is fundamentally different from forgiving a loved one.
- Decisional and emotional forgiveness are different processes:
- Decisional forgiveness involves a decision to control one’s own behaviors (e.g., not to engage in activities that increase anger or create contact with the offender). Decisional forgiveness has the “potential” to lead to changes in emotion and eventually behavior.
- Emotional forgiveness is multifaceted and involves changes in cognition, emotion, motivation, and eventually behavior.
There is a substantial body of research supporting a relationship between hostility and poor health; for example, hostility is linked to heart disease and all-cause, general mortality.[63] Forgiveness, on the other hand, has been associated with many benefits, including:[219]
- A reduced risk of all-cause mortality[220]
- Improved mental health, reduced negative affect or emotions, and increased well-being.[64-67]
- Decreased stress levels and mental health symptoms.[68]
- Satisfaction with life[67,69]
- Fewer physical ailments, less medication use, reduced fatigue, better sleep quality, and fewer somatic complaints[70]
- Reduced levels of depression, anxiety, and anger[64,67,71]
- Reduced risk of myocardial ischemia and lower total cholesterol to HDL and LDL to HDL ratios among patients with coronary artery disease[72,73] and decreased cardiovascular reactivity[74]. Forgiveness lowers blood pressure.[221]
- Self-forgiveness was associated with lower levels of disordered eating behavior.[75]
- Reduction of vulnerability to chronic pain[76,77], including from fibromyalgia symptoms[222]
- Decrease in vulnerability to use illicit drugs at post-test and four-month follow-up for substance abusers[78]
- Improvement in immune function at the cellular level.[223]
- Decreased stress at work, especially with forgiveness practices focused on coworkers[224]
- Improved hope and quality of life in people with terminal cancer[225]
- Forgiveness related to an adverse childhood experience in a parent duces the chances that their children will experience those same experiences.[226]
Of course, one need not have a specific diagnosis or health problem to make use of forgiveness as a self-care practice. It can be beneficial to everyone.
Enright and Fitzgibbons outlined four stages of forgiveness.[79]
- Uncovering
This can include processes such as the following:
-
- Gaining insight into the injustice and subsequent injury and how it has compromised one’s life
- Confronting anger and shame
- Becoming aware of potential emotional exhaustion
- Becoming aware of cognitive preoccupation
- Confronting the possibility that the transgression could lead to permanent change for oneself, including altering the one’s view of the world
- Decision
Gaining an accurate understanding of what forgiveness is, and making a decision to commit to forgive on the basis of this understanding
- Work
Gaining a deeper understanding of the offender and beginning to view the offender in a new light (reframing), resulting in positive change in affect about the offender, oneself, and about the relationship
- Deepening
Finding meaning in the suffering (post-suffering growth)[80,81]
For more information on forgiveness, go online to the Whole Health tool “Forgiveness: The Gift We Give Ourselves.”
Gratitude
Fredrickson states “gratitude and other positive emotions fuel individual growth, development, and resilience.”[80] Gratitude involves noticing and appreciating the positives in life. It is commonly derived from receiving aid from another, an appreciation of abilities, or being in a climate in which one can thrive.
Gratitude is universal and found across all cultures and all people. It is considered a virtue and is different from optimism, hope, and trust.[82] The root of the word gratitude is the Latin root Gratia, which means “grace, graciousness, or gratefulness...all derivatives from this Latin root having to do with kindness, generousness, gifts, the beauty of giving and receiving, or getting something for nothing.”[82]
Gratitude practices studied by research are classified into three categories[81]:
- Listing of things for which one is grateful
- Grateful contemplation
- Behavioral expressions of gratitude
Empirical research has found that gratitude can improve a person’s sense of personal well-being in two ways[82]:
- As a causal agent of well-being
- Indirectly, as a means of buffering against negative states and emotions; that is, gratitude makes us more resilient to stress
A number of researchers have proposed a theoretical relationship between gratitude and well-being. Experiencing gratitude, thankfulness, and appreciation tends to foster positive feelings, which in turn contribute to one’s overall sense of well-being.[82,83]
Gratitude has been linked to a host of psychological, physical and social benefits:
- Improved self-reported physical health[84]
- Feeling more happiness, pride, and hope [85]
- Increased life satisfaction[227]
- Decreased suicidal ideation in Veterans[228]
- A greater sense of social connection and cooperation; feeling less lonely and isolated[86] and better able to maintain intimate bonds.[87]
- A reduction in risk for depression, anxiety, and substance abuse disorders[88,229]
- Increased self-efficacy for family caregivers of people with mental illnesses[230]
- Improvement in body image[89]
- More acts of kindness, generosity, and cooperation[90,91]
- Greater resilience in the face of trauma-induced stress, recovering more quickly from illness, and enjoying more robust physical health[92]
- Improvement in sleep and energy[93]
- An association with improved cognitive function in older people[231]
- Decreased cardiovascular disease risk[232]
- Improved palliative care experiences and outcomes for people with cancer and their families[233]
- Decreased prejudice among groups[234]
A 2021 review connected trait gratitude (and optimism) with “lower heart rate and blood pressure, better sleep, more exercise, less stress, more positive expectations and reflections, and greater feeling of appreciation toward others.”[235]
For more information on gratitude, refer to the “Creating a Gratitude Practice” Whole Health tool.
Random Acts of Kindness
A random act of kindness is defined as something a person does for an unknown other, that he or she hopes will benefit that individual.[94] Examples include paying for the order of the person behind you in the drive through, putting money in a parking meter for someone whose meter has expired, and giving a stranger a flower.
Kind acts have been found to positively correlate with enhanced life satisfaction.[95] Lyubomirsky and colleagues conducted two 6-week-long interventions where participants performed five kind acts in one day every week.[31] Participants experienced an increased sense of happiness, an effect not found in the control group.
Buchanan and Bardi conducted an experiment where participants performed new acts of kindness every day for 10 days and found it increased life satisfaction compared to a control group.[94]
FMRI scans show that even the act of imagining kindness or compassion activities activates the soothing and affiliation parts of the brain’s emotional regulation.[96] Kindness, therefore, can become a self-reinforcing habit requiring less effort over time to engage in and creating new neural connections.[97] Creating and encouraging a culture of kindness in health care can be an effective way to promote resilience and provide a buffer against stress and burn-out.[98] More research is needed to gauge the degree of benefit that random acts of kindness, and in what situations.[236]
It can help to strategize in advance about what specific acts of kindness one could perform. Some research indicates that people underestimate the value their acts of kindness will have on others.[237]

Mindful Awareness Moment
A Random Act of Kindness
This mindful awareness exercise takes a bit more than a “moment” to complete. Start by taking a moment right now to consider what you could potentially do for another person as a “random act of kindness.” How do you feel as you imagine following through with one of the acts that comes to mind?
Now, sometime in the next 24 hours, perform an act of kindness, and when you have finished, ask yourself the following:
How did I feel as I did it? (If you did not do it, why was that?) Did I feel nervous? Excited? Sheepish? Happy? Something else?
Did it feel the way I anticipated it would feel?
Repeat this exercise as often as you would like. You might even try performing a random act of kindness for yourself.
Humor & Laughter
The old man laughed out loud and joyously shook up the details of his anatomy from head to foot and ended by saying that such a laugh was money in a man’s pocket, because it cut down the doctor’s bills like everything.
—Mark Twain, Tom Sawyer
Humor, if utilized in the right way, can help to relieve stress in the workplace and at home. It can even, perhaps, help with pain. Humor is a reactive experience, and most definitions of it draw in elements of unexpectedness, surprise, anticipation, incongruity, or incompatibility.[99] Sense of humor is highly individualized; therefore, gender, age, ethnicity, etc., need to be considered. The study of humor and laughter, and its psychological and physiological effects on the human body, is called gelotology.
There are multiple known benefits of laughter and humor, and the amount of research in this area is rapidly expanding:
- A 2024 systematic review of 18 studies concluded that there is a positive association between various facet of humor, such as humor style, sense of humor, and laughter, and quality of life in people with chronic diseases.[238]
- A 2022 meta-analytic review of 45 studies with 2,547 participants concluded that “Laughter -inducing interventions can have beneficial effects on a variety of health-related outcomes including mental health, physical health, and physiological parameters.”[239]
- In a study of 240 people with rheumatoid arthritis, how much a person laughed in a given time period was favorably associated with level of depression and frailty.[240]
- During laughter, various muscle groups are activated for periods of seconds at a time, while the period immediately following a laugh leads to general muscle relaxation that can last up to 45 [100]
- Engaging in intense laughter leads to increased heart rate, respiratory rate, and oxygen consumption—similar to physiological changes noted in aerobic exercise.[101]
- Earlier research examining how laughter influences stress hormones has shown conflicting results,[102,103] but a 2023 meta-analysis concluded, using 8 studies with 315 participants, that spontaneous laughter does decrease cortisol levels compared to usual activities. Some studies conclude that laughter decreases stress hormones and may act as a buffer to the effects of stress on the immune system.[104-106]
- Researchers found that older patients who completed a Humor Therapy program had significant decreases in pain and perception of loneliness. There were significant increases in happiness and life satisfaction in the experimental group but not for the control group.[107]
- In a systematic review of the literature, these reviews found that humor undoubtedly has a role in palliative care but requires training for its appropriate use.[108]
- Humor may relieve self-reported stress and arousal.[106]
- A sense of humor appears to be part of the multifaceted and multicomponent experience of wisdom.[111]
- People who laugh more seem to have better oral health and keep their teeth longer.[241]
- Having more occasions for laughter was found in a 6-year cohort study to be tied to a lower risk for developing dementia.[242]
- There is increasing evidence to suggest that simulated laughter (Laughter Therapy or laughter yoga) has a variety of benefits.[109,110]
- Laughter therapy is beneficial as a supportive therapy in palliative care, decreasing mood disturbances and caregiver burnout levels.[243]
- A 2023 meta-analysis of 7 studies found laughter therapy improves negative emotions in cancer patients.[244]
- or people with type 2 diabetes, laughter therapy delays the onset of complications of diabetes, enhance cardiovascular function, and rectify abnormal homeostasis.[245]
- Laughter therapy increased quality of life for people with schizophrenia, with benefits related to other measures such as optimism, coping, sociability, motivation, and functionality as well.[246]
- In Japan, a 12-week laughter intervention program, mostly laughter yoga, improved body weight, BMI, subjective stress, well-being, and quality of life in elderly people.[247]
- A 12-week laughter yoga program was linked to better glycemic control in people with type 2 diabetes (0.31 improvement in A1c).[248]
- A Turkish study found benefits of and 8-session laughter yoga class for resilience, loneliness level, and quality of life in older adults.[249] A study of 66 retired Iranian women found improvements in anxiety and depression.[250]
- A study of 80 women with premenstrual symptoms found significant benefits for many subdimensions with laughter yoga.[251]
- Laughter yoga had a positive impact on happiness and stress for nursing students starting clinical practice.[252]
- Laughter yoga showed promise for reducing chemotherapy-induced nausea in a randomized trial involving 69 cancer patients.[253]
- For a group of 84 Chinese patients with lung cancer receiving chemotherapy, laughter yoga had beneficial effects on stress, psychological capital, and exercise capacity.[254] An Iranian study also found benefits for 69 patients with a variety of cancers.[255]
- Laughter yoga improved resilience and sleep quality in a study of 90 Turkish nurses during the COVID-19 pandemic.[256]
- Clown therapy reduces anxiety and procedural pain in children.[257]
- Laughter yoga improved pregnancy symptom frequency and prenatal attachment in a group of 85 pregnant women.[258]
- Laughter yoga helped sleep quality in people with fecal ostomies.[259]
- Laughter yoga improved sleep quality and reduced pain in a study of 68 people receiving hemodialysis.[260]
Formed in 1987 by a registered nurse, the Association for Applied and Therapeutic Humor (AATH) is a nonprofit, member-driven, international community of humor and laughter professionals and enthusiasts. To learn more, go to the AATH website.
For additional information, refer to “The Healing Benefits of Humor and Laughter” Whole Health tool.
Creativity
The American Psychological Association defines creativity as “...the ability to produce or develop original work, theories, techniques, or thoughts,” noting that creative individuals show expressiveness, imagination, and originality and can innovate in a variety of ways.[261] Trunell and colleagues identify four characteristics of creativity[112]:
- Supportive environments and intrinsic (inner) motivation enhance creativity.
- Intrinsic motivation, which enhances creativity, is itself enhanced by the completion of tasks.
- Creativity involves both divergent and convergent thinking.
- Divergent thinking promotes the generation of many new ideas. An example is brainstorming all the possible uses for a paperclip.
- Convergent thinking focuses on finding the solution to a particular problem. For example: What do a horse, plane, and boat have in common? (They are all forms of transportation.)
- Analogies and metaphors enhance creativity.
A 2023 meta-analysis concluded that mindfulness can be used as a tool to enhance creativity.[262] Colzato and colleagues found that practice of a type of meditation called “Open Monitoring,” during which a practitioner is receptive to all thoughts, sensations, experiences, and emotions without singling anything out, appears to generate more new ideas for the intervention group, as compared to controls. [113] Note that creativity can have a “dark side,” too; what is created may cause adverse outcomes.[263]
A 2010 meta-analysis demonstrated that a lack of control significantly stifles creativity.[114] The same meta-analysis noted that creativity and stress have a complex relationship that cannot be simplified down into exclusively positive and negative impacts.[114] Openness to Experience is a key personality trait linked to creativity.[264] Trust is important to the creativity of both individuals and groups.[265]
What happens with the creative process at the neuronal level is not clear, but one possibility is that creativity is associated with slow, spontaneous fluctuations in the activity of neurons.[266] Dopamine has been associated with increases in creativity, and genetics research on creativity has begun to emerge.[267-269]
To increase creativity, research suggests the following:[115,116]
- Use an idea notebook, voice recorder, or even a napkin in a restaurant to capture ideas when they arise.
- Surround yourself with things, events, and people that are interesting or novel, to stimulate new thinking.
- Broaden your knowledge base by taking a class or learning something outside your area of expertise. This makes more diverse knowledge available for interconnection during the creative process.
- Seek out challenging tasks that might not even have a solution. This causes old ideas to compete with each other and helps generate new ones.
- If you are trying to solve a problem, sleep on it. One study suggested that sleep may help problem-solving and that solutions may even come in the form of a dream. [117]
In medical school, creative writing has been suggested as a means to “...promote not only self-expression and self-awareness, but also the ability to observe, listen, and empathize” for the physician in training.[118] This self-awareness, or ability to reflect, is also discussed in the lifelong learning section of this module. For detailed information, refer to the “Narrative Medicine” Whole Health tool.
Work-life Balance
The concept of work-life balance emerged in the 1970s and 1980s as more women moved into the workforce, and the concept has continued to evolve with societal changes related to gender roles, technology, and the ways that work is done in the 21st century.[270] The term “work-life balance” implies that work is not a part of “life,” or perhaps that work has to be time spent doing something negative, which is not necessarily true for many people. As Swiss philosopher Alain de Botton put it, “There is no such thing as work-life balance. Everything worth fighting for unbalances your life.”[i] Recently, people have begun to use the term, “work-life integration” or even “work-life blend,” given that it is now possible with technology to take work with us wherever we go.
Most of the literature on this topic can nonetheless still be searched using the term “Work-Life Balance.” Work-life balance was defined by Hill and colleagues as “the degree to which an individual is able to simultaneously balance the temporal, emotional, and behavioral demands of both paid work and family responsibilities.”[119] It has been defined by Streu et al. (2011) “as the perceived sufficiency of time available for work and social life.”[120] It has also been defined more broadly as maintaining an overall sense of harmony in life.[121] Cultivating work-life balance is an iterative process that involves acknowledging, adapting, and adjusting personal priorities and situations in response to a myriad demands. What balance means to an individual will change depending on their personal and career situations and involves constant reassessment and decision-making depending on evolving factors in both work and life; like so many aspects of a person’s whole health, it is in some ways unique to each individual.[122]
A joint report from the Center for American Progress and the Center for Work Life Law at the University of California Hastings College of the Law found that 90% of mothers and 95% of fathers report work-family conflict.[123] Failure to achieve balance between work and home life has been associated with reduced job and life satisfaction, impaired mental health, family conflict, and ultimately burnout.[124]
Chittenden and Ritchie identify the following five strategies one can follow to enhance work-life balance:[125]
Strategy 1: Work with time-shifting and mindful awareness
This is the ability to “downshift,” to develop an awareness of the body using mindful awareness or awareness of thoughts and sensations one experiences in the present moment. This practice allows one to feel that time slows down. This reduces stress, increases happiness, and makes a person more efficient.
Strategy 2: Set goals
Goals should be guided by personal values. One method involves writing down 10 long-term goals every day for a week. At the end of the week, identify the 10 goals that most consistently appear in the daily lists. Then write down the steps to make each of these 10 major goals possible, breaking them down into yearly, monthly, weekly, and even daily tasks. It can be helpful to also write a personal vision or mission statement to set clear priorities both professionally and personally. An important step is to regularly monitor how these goals are being met. This can lead to clarification about goals (are they unrealistic?), about oneself (what factors could be getting in the way?) and about one’s values (are these goals truly aligned with my personal values?). See the “Values” Whole Health tool for more information.
Apply the principals of SMART goals (a few at a time) to focus on how to reach each goal. For more on how to set SMART goals refer to the tool in Chapter 3 of the Passport to Whole Health. SMART stands for:
- Specific
- Measurable
- Action-Oriented
- Realistic
- Timed
Strategy 3: se cognitive reframing and build resilience
Another way to improve work-life balance is to become aware of common cognitive distortions that get in the way at work, home, and in finding the balance between these two. Identifying these negative messages and learning how to counter these distortions with more balanced thoughts is a powerful tool in problem-solving and making positive changes. Some common cognitive distortions include:[271]
- Jumping to conclusions
- Catastrophizing
- Personalization
- The fallacy of fairness
- Discounting the positive
A person can use mindful awareness to monitor cognitive distortions they use, so that you can reframe their thoughts.
Strategy 4: Practice self-care
Make time for self-care through exercise, adequate sleep, healthy eating, and the other aspects of self-care featured on the Circle of Health. Finding ways to nurture oneself emotionally and spiritually and to nurture relationships with spouses/partners, children, friends, and family are vital. Engaging in the larger community, and spending time in self-reflection though regular prayer, meditation, and reflective journaling are also components of self-care.
Strategy 5: Ask for help
Find ways to protect time for family and self by asking for help with daily-living activities, as well as with emotional and spiritual issues. Seek help from work colleagues or mentors when feeling overwhelmed and at risk for burnout.
Additional information is provided online in the “Work-Life Integration: Tips and Resources” tool.
Lifelong Learning
Anyone who stops learning is old, whether at twenty or eighty. Anyone who keeps learning stays young. ― Henry Ford
All the world is my school and all humanity is my teacher. ― George Whitman
With the rapid pace of technology and scientific research, we all stand the risk of becoming out-of-date if we do not continue reading and studying during our careers.[126] In lifelong learning, emphasis is placed on the development of learner capacity, autonomy, and capability. The goal is to produce learners who are well-prepared for the complexities of today’s workplace.[127] Distance learning is an example of a type of learning that promotes learner autonomy in the rapidly expanding field of technology.
Lifelong learning means striking the “...right balance between confidence and doubt.”[128] For professionals, this includes continuing to question their actions and knowledge through self-reflection and self-assessment throughout their careers. Professionalism has its core in a commitment to lifelong reflection, self-assessment, and improved performance through learning.[129]
A meta-analysis that included medical students, residents, and practicing health professionals showed that if an orientation toward lifelong learning was high, it continued to grow, even after the completion of formal education or training.[129] Modern clinical practice fundamentally requires lifelong learning and self-reflection, according to Stephenson and colleagues.[130]
A lifelong learner has the following qualities:
- Flexibility to change based on practice demands
- Awareness of the need for lifelong learning
- Encouragement of peer review of their work
- The ability to share good practice and knowledge (e.g., in medicine, through grand rounds, journal clubs, etc.)
- Keeping a reflective diary and reading relevant journals for ideas for improving practice
- A high level of motivation that allows them to be a change agent
- Willingness to be challenging and creative in their work, engaging with colleagues and peers
- Abilit to effectively use resources to support making improvements
Research shows that education is another powerful social determinant of health and well-being. There is an association between adult education and midlife cognitive ability, including verbal ability, memory and fluency. [132] There is also a link between educational attainment and leukocyte telomere length (LTL), according to a study in the United States where higher education appeared to have a protective benefit against telomere shortening (a measure of accelerated cellular aging).[133]
Education promotes problem-solving skills, leading to reduced biological stress response, with favorable consequences for biological aging and well-being.[134,135] Educational differences in mortality have been explained to a significant degree by the strong association between education and income.[136] Americans' education and income levels are highly correlated with each other. Furthermore, there appears to be an inverse relationship between all-cause mortality and years of education.[137] Higher education is one of the most effective ways that parents can raise their family’s income.[138] Of note, some studies have found that higher educational attainment was connected with better mental health but decreased physical health for people from economic disadvantage, highlighting that the relationship between education and health is complex.[272] Attending ‘higher-quality colleges’ may correlate with better physical health but not mental health long-term.[273]
Take time to ask, as part of the Whole Health approach, what people are learning, as well as what their educational goals currently are.
Leisure & Hobbies
Life away from work has an impact on how people feel and behave at work.[139] Vacations and periods of rest decrease perceived job stress and burnout[140,141] and increase life satisfaction.[140] However, vacation effects fade quickly, and well-being deteriorates soon after a person returns to work.
Thus, individuals need additional opportunities for recovery and recharging from work in the evening and/or during weekends. Setting aside time for leisure activities is an important strategy for coping with stress and negative life events. Leisure has been defined as unobligated time, away from work, personal maintenance, evaluation, and judgment, during which freely chosen and intrinsically motivated activities, both active and passive, social and solitary, are pursued for enjoyment and relaxation toward achieving a state of mind that supports rejuvenation, and contributes to overall quality of life, health, and well-being.[142]
Recovery attained during leisure time has an effect on the following:
- How individuals experience the subsequent workday[139]
- Overall well-being[139]
- Prevention of burnout[143]
- Inhibiting ongoing deterioration in mood and performance over the long term[144]
Engagement in meaningful life activities produces a sense of satisfaction and a belief that life is being well-lived.[145] It is strongly correlated with happiness, too.[31] Lyubomirsky and colleagues note that putting sustained effort into doing these happiness-enhancing activities, rather than doing them for only a week, is essential to their beneficial effects. Repeated effort at cultivating happiness through meaningful life activities can relieve symptoms in mild to moderately depressed individuals and outpatients with major depressive disorder and other affective disorders.[28,146,147]
Leisure experiences, such as engaging in hobbies, can aid in coping with induced stress in ways that are self-protective, self-restorative, and ultimately personally transformative.
Kleiber and colleagues propose the following mechanisms by which leisure is an effective strategy for coping with the stress created by negative life events"[148]:
- Buffer the impact of negative life events by being distracting
- Decrease the impact of negative life events by generating optimism about the future
- Aid in the reconstruction of a life story that is continuous with the past
- Serve, in the wake of negative life events, as vehicles for personal transformation
Participation in leisure activities is also associated with various components of successful aging, including physical health and well-being.[149] Research by Paggi, Jopp and Hertzog (2016) highlighted the importance of leisure activities for successful aging throughout the adult life span.[150] They encouraged engaging in leisure activities that correspond with the level of physical ability throughout life to maintain and even improve well-being.
The online Whole Health tool “Taking Breaks: When to Start Moving, and When to Stop,” has more information on vacations, leisure time, and work breaks.
Volunteering
In 2023 about 63 million people volunteered regularly. This is nearly 25% of the U.S. population.[274] In 2019, the value of volunteer work was estimated to be over $167 billion. At the height of the pandemic, 51% of the US population over age 16 reported helping their neighbors.[275] Veterans volunteer more than the general population.[274] Research provides strong evidence that volunteering has not only social benefits, but positive health benefits as well. The 2007 report, “The Health Benefits of Volunteering: A Review of Recent Research” described a significant association between volunteering and health.[151] This report, along with other, more recent studies, indicates that volunteers have:[276-280]
- Greater longevity
- Better functional ability
- Lower rates of depression, frailty, and loneliness (known to be a significant risk factor for many health problems) in later life
- Less incidence of heart disease and lower
- Improved cognitive functioning and slower cognitive decline
- Decreases in inflammation (e.g., levels of C-reactive protein)
In addition to volunteers having improved physical and mental health, they are found to have greater life satisfaction and quality of life. [152,153]
Research has found that volunteering has a positive effect on other social and psychological factors as well, such as [154,155]:
- Increasing a personal sense of purpose and accomplishment
- Enhancing social networks to reduce stress and risk of disease
Research by Clay found that volunteering serves a variety of functions, including the following[156]:
- Acting on values: The individual volunteers to express or act on important values like humanitarianism.
- Gaining understanding: The volunteer is seeking to learn more about the world or to exercise skills that are often unused.
- Enhancement: One can grow and develop psychologically through volunteer activities.
- Career advancement: The volunteer has the goal of gaining career-related experience through volunteering.
- Social benefits: Volunteering allows an individual to strengthen his/her social relationships.
- Skill-building: The individual uses volunteering to reduce negative feelings, such as guilt, or to address personal problems.
Other studies have found that when individuals with chronic or serious illnesses volunteer, they receive benefits beyond what can be achieved through medical care alone. However, a “volunteering threshold” was found; after this threshold was reached (i.e., volunteering in two or more organizations or volunteering more than 100 hours/year), no additional health benefits occurred. [157,158]
A 2011 review of studies conducted by von Bonsdorff and colleagues highlighted several benefits of volunteering.[159] Outcomes were collapsed into three areas of personal well-being: physical health, mental health, and psychosocial resources. All included studies came from the United States, and all found that volunteering in old age predicted better self-rated health, functioning, physical activity, and life satisfaction; depression and mortality were decreased.
An analysis of the experience of more than 1,700 women who were involved regularly in helping others had these effects[160]:
- 50% of helpers reported a “high”
- 43% felt stronger
- 22% felt calmer and less depressed
- 13% had fewer aches and pains
- 21% had a greater feeling of self-worth
Of the participants, 72%-80% stated that these benefits, such as their helper’s high, would reoccur, though with less intensity, when they remembered helping. The authors stated that the pleasure one receives from being altruistic and volunteering does not seem to arise from donating money, no matter how important the cause, nor from volunteering that occurs without close personal contact.
Financial Health
Financial health often refers to the state of a person’s financial life or financial situation. It is a general term that could include a variety of topics, such as the amount of savings someone has (e.g., retirement, savings account funds, or college savings), how much income is spent on fixed or nondiscretionary expenses such as rent or mortgage, ability to pay debts, etc. Another oft used term is “financial literacy,” which is defined as the ability to make informed judgments and manage money effectively.[174]
Financial debt and health
Recent data suggests that those with medical or credit card debt may forego prescription medication prescribed by their clinician, even when net household income, net worth, and other characteristics are taken into account.[186] In a survey conducted by the American Psychological Association, nearly 1 in 5 Americans say that they have either considered skipping (9%) or skipped (12%) going to the doctor when they needed health care because of financial concerns. A systematic review and meta-analysis also found association between debt and health, with more severe debt being related to worse health; however causality is hard to establish.[187]
Does more money make us happy?
Research has suggested that there is a small but positive association between income and happiness. However, this relationship is not linear; the positive associations between money and happiness decreased significantly at higher levels of income.[175,176] Happiness and income appear more highly associated at lower levels of income, with decreasing effect once income exceeds poverty level.
Financial debt and health
Recent data suggests that those with medical or credit card debt may forego prescription medication prescribed by their clinician, even when net household income, net worth, and other characteristics are taken into account.[177] In a survey conducted by the American Psychological Association, nearly 1 in 5 Americans say that they have either considered skipping (9%) or skipped (12%) going to the doctor when they needed health care because of financial concerns. A systematic review and meta-analysis found association between debt and health, with more severe debt being related to worse health; however, causality is hard to establish.[178]
Money and stress
Financial health and literacy can be a source of stress. The American Psychological Association (APA) conducted a survey and found that stress associated with finances and money is widespread.[179] In fact, 72% of Americans report that finances are a significant cause of stress, and this seems especially true for parents and younger adults. The report suggests some tips to manage financial stress[180]:
- Pause but do not panic. Panic and anxiety can lead to poor decision-making. It is important to avoid overreacting or becoming passive about finances. Remain calm and stay focused.
- Identify financial stressors and make a plan. Assess financial health and take note of what creates stress. Commit to a specific plan and review it regularly. Facing financial stress can create more anxiety in the short-term, but putting things down on paper and committing to a plan can reduce stress in the long-term.
- Recognize how one deals with stress related to money. Financial stress can cause a person to engage in activities that create more stress, such as smoking, drinking, gambling, emotional eating, etc. These negative coping techniques can add to stress in family and partner relationships.
- Turn challenging times into opportunities for real growth and change. Economic challenges can motivate one to find healthier ways to deal with stress. Use financially challenging times to think outside the box and explore new approaches.
- Ask for professional support. Credit counseling services and financial planners are available to help people gain control over their financial situation.
The American Institute for Research (AIR) conducted a review of the literature and found that financial education and counseling are closely connected to financial health in many ways.[174] Better long-term financial outcomes are associated with highly targeted and proactive counseling. Education assists in managing present difficulties and in preventing future problems. Ongoing peer mentoring, interactive assistance, counseling, and coaching can be crucial in helping consumers attain long-term goals such as financial stability.
The U.S. Department of Health and Human Services, through its 2009 Healthy Relationships and Financial Stability project, developed the following 10 suggestions for healthy family finances[181]:
- Set common financial goals and formulate steps toward them.
- Regularly discuss financial and other goals at home.
- Involve all family members, including children, in the plan.
- Avoid schemes with high hidden fees, like check cashing stores (use banks instead), rent-to-own schemes (wait and buy), or certain credit cards.
- Pay yourself first. Put something in your account for your future even as you pay others for their services.
- Communicate when there is conflict, including with companies to whom one owes money.
- Check credit reports regularly including those of a spouse or partner. These can be ordered for free.
- Make sure the family receives Earned Income Tax Credit (EITC) and any other government benefits for which they qualify.
- Know when to seek assistance. Pivotal moments that affect finances include getting married, getting divorced, having a baby, or adopting a child.
- Know that there are resources available to help, regardless of one’s current financial and family situation.
financial health Resources
- Money Smart
- Financial education program created and run by the Federal Deposit Insurance Corporation (FDIC). Money Smart materials are free and can be ordered on the FDIC’s website.
- Financial Knowledge Institute
- Nonprofit educational organization that specializes in onsite workshops on personal financial topics. The speakers are community members who donate their time to share their passion of creating financial literacy.
- Institute for Financial Literacy
- Nonprofit organization whose mission is to promote effective financial education and counseling.
- Money Management International
- S. network of nonprofit agency that provides free professional credit counseling, debt management programs, and consumer education.
- National Endowment for Financial Education
- Information on ways to save money, tips on how to become a savvy saver, a savings quiz, and financial calculators to help figure out how long it would take to save money or pay off a loan.
- Take Charge America
- Nonprofit organization that provides education, counseling, and debt management.
- My Money
- Information from the U.S. Government to help improve the financial literacy and education of persons in the United States.
- Women’s Institute for Financial Education
- WIFE is a nonprofit organization which provides financial education and networking opportunities to women of all ages.
- The American Financial Services Association Education Foundation (AFSAEF)
- An affiliate of the American Financial Services Association (AFSA) is a nonprofit organization to heighten consumers' awareness of personal financial responsibility. AFSAEF's mission is to help consumers realize the benefits of responsible money management, understand the credit process, and seek help if credit problems occur.
- Consumer Financial Protection Bureau
- Provides consumers answers to questions about financial products and services, including credit cards, mortgages, student loans, bank accounts, credit reports, payday loans, and debt collection.
Back to Sarah
During her Whole Health visit, Sarah spoke at length with her primary care clinician, and later with other members of her clinical team, about Personal Development, which emerged as a priority among the various components of proactive self-care (the green part of the Circle of Health). Her PHI made it clear that she has a lot of good ideas. When co-creating her Personal Health Plan (PHP) with her team, Sarah noted that she could set (over time, so as not to be overwhelmed) several Personal Development-related goals:
- Quality of work life
Sarah is doing well with this. She has great relationships with her colleagues and enjoys what she is doing. She will do more reading about burnout, as she knows she is at risk of this given that she takes care of a number of seriously ill people as a certified nursing assistant.
- Resilience
She could review information on enhancing resilience and will focus on at least one thing that will help her to have a greater sense of meaning and purpose in her life.
- Happiness
She recognizes that happiness matters a lot to her, but she has not been particularly happy since her divorce. She intends to work on that, mainly through reconnecting with her old church congregation and spending at least one night a week having family game night with her kids and their friends.
- Hope and optimism
Sarah feels optimistic overall and will continue to model that for her children.
- Self-compassion
Sarah could begin a routine Mindful Self-Compassion practice.
- Forgiveness
She will review the “Forgiveness: The Gift We Give Ourselves” tool and start working on this in terms of how she feels about her ex-husband. She was relieved to learn forgiveness was in no way about condoning any of his past behaviors.
- Gratitude
Sarah could identify three things she is grateful for every day as she drives home from work.
- Random acts of kindness
Sarah notes that she performs these frequently in her healthcare work and can explore novel ones she has not tried before.
- Humor and laughter
Sometime down the road, perhaps in a month or two, she hopes to do a laughter yoga session with her care team at the hospital.
- Creativity
She can begin scrapbooking again.
- Work-life balance
While this is challenging for her, given all her obligations, she could take 20 minutes a day just for herself. She will check in with her clinical team about how that is going after two weeks.
- Lifelong learning
Sarah is already planning to attend nursing school.
- Leisure time and hobbies
She could start scrapbooking and having family game night, as noted above.
- Volunteering
Sarah does not have a lot of time for this right now, but she understands it can have health benefits and notes she could have her kids volunteer with her at an upcoming church activity.
- Social capital
Sarah could host dinner at her house for her family and friends at least three times a year. After exploring her values, Sarah wants to create a family tradition of taking a walk together after Sunday dinner.
- Financial health
She could find an affordable financial advisor and has access to the resources listed at the end of the Financial Health section of this module. She spent an afternoon a few weeks ago on a free financial website to create a family budget. Although it is not working perfectly, she worries less because she has come up with a plan.
During Sarah’s visit with her clinician, one of their main tasks was decide on priorities, so that she would not be overwhelmed by the list of possible actions she could take. Ultimately, she decided to start with more time with her kids (scrapbooking, nature time together, and other family time) and spending more time at church to build friendships and incorporate some volunteer opportunities. She will follow up with a member of her care team in one month to explore other options.Resources
Whole Health Tools
Author(s)
This overview was written by Shilagh A. Mirgain, PhD and Janice Singles, PsyD and updated by Adam Rindfleisch (2014, updated 2024).
This Whole Health overview was made possible through a collaborative effort between the University of Wisconsin Integrative Health Program, VA Office of Patient Centered Care and Cultural Transformation, and Pacific Institute for Research and Evaluation.




















Social Capital
The term “social capital” was first introduced at length by Robert Putnam in his national bestseller, Bowling Alone: The Collapse and Revival of American Community.[161] The act of bowling alone was used as a reference to the disintegration of U.S. after-work bowling leagues as a metaphor to illustrate the decline of social, political, civic, religious, and workplace connections in the United States.
Social capital refers to various levels of social relationships formed through social networks. It is a complex phenomenon that is the result of social relationships based on reciprocal exchanges between family and friend networks; co-workers; members of social, religious, or political organizations; and residents in the same neighborhood. It can improve the efficacy of a society by facilitating coordinated actions.[162] The core idea is that social networks have value. Similar to physical and human capital, social contacts can increase the productivity of individuals and groups.
People create connections with each other, and these connections are important in a variety of ways. In a classic example of social capital, people who attend the same university usually feel connected with each other, both because they may have formed a friendship attending school together and/or because they share an institution in common. Two graduates of the same university are more likely to connect with each other and provide information or resources because they share social capital.
Other examples of settings where social capital arises include a community garden, a neighborhood running a neighborhood watch program, a church congregation, or people who work out at the same local gym.
A 2014 meta-analysis by Gilbert and colleagues focused on social capital research and found a strong positive relationship between social capital and health as measured by self-reported health and mortality.[163] Kawachi and Berkman conjectured that social capital provides opportunities for psychosocial support which, if accessed, will tend to reduce stress and improve health.[164] Berkman and colleagues suggest that social capital influences health through different pathways.[165] First, social support allows a person to feel cared for and that they belong to a network. Second, there is influence through shared norms. Third, there is social engagement and participation, and lastly there are person-to-person contacts, which are especially pertinent in certain behaviors, such as secondhand cigarette smoking or shared food and beverages.
One study found that social capital at work, having strong social ties with co-workers and a work environment that values and fosters social connections, reduced risks of burnout.[166] Research suggests that low levels of social capital may also negatively impact the quality of care provided for patients, whereas high levels of social capital contribute to increased employee satisfaction and engagement and positive work environment.[167-172] Additionally, a study conducted in 15 healthcare settings explored the mediating role of social capital between job performance and employee engagement and recommended facilitating social capital to increase employee performance.[173]
Hofmeyer and Marck (2008) recommend fostering social capital in modern healthcare systems in five dimensions:
Refer online to the “Family, Friends, & Co-Workers Whole Health overview for more information on how to increase social capital.