Journeys with High Blood Pressure
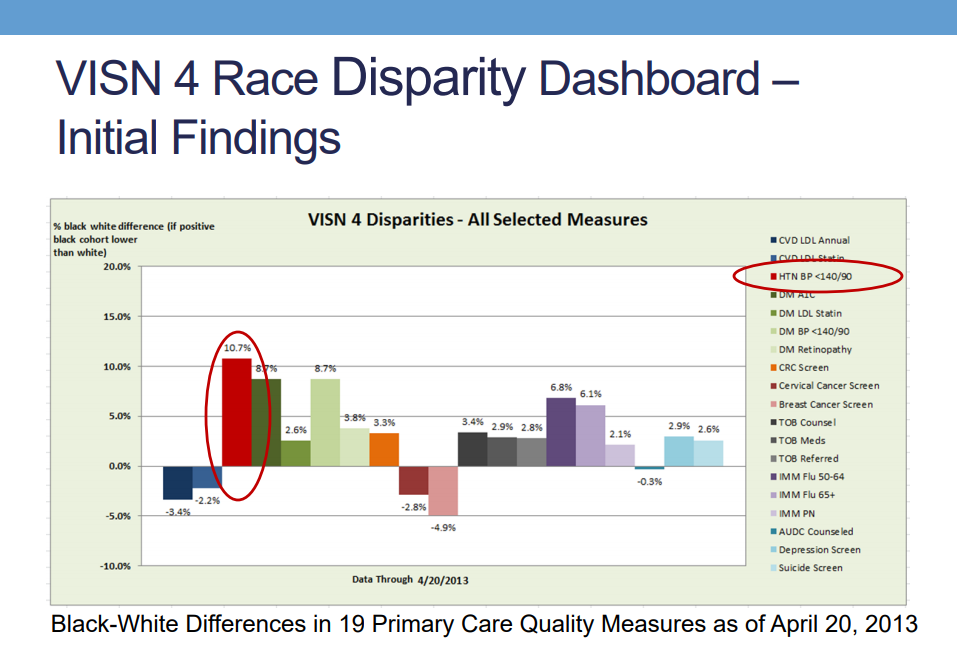
Did you know that some Veterans, including some racial and ethnic minorities, experience higher rates of hypertension? A
VA research team created a series of videos of patients discussing their experiences with high blood pressure and offering tips to take medications, talk to their health care providers, and make other changes. According to the
2016 study, Veterans who watched the videos, compared to those who did not watch the videos, reported greater intentions to:
- Become more physically active;
- Use salt substitutes;
- Talk openly with their doctor about hypertension; and
- Remember to take their hypertension medications.
The Office of Health Equity is pleased to be able to share these videos with Veterans and stakeholders. The short videos below feature stories from Veterans about high blood pressure and important resources.
Module 1 - Journeys with High Blood Pressure
 Introduction
Introduction
Natasha, an Army Veteran who served for 7 years and worked as a medic, highlights the importance of managing high blood pressure in the African American community. Natasha introduces five African American Veterans who successfully manage their blood pressure. As these Veterans share their stories, Natasha reflects on key factors in their journeys that may help you.
 Danny
Danny
Born and raised in Charleston, South Carolina, Danny shares how the eating habits he developed growing up in the South and while serving in the military lead to his weight gain as a retiree since he no longer exercised daily like a soldier. Eventually, Danny had an episode of blurred vision, was admitted to the emergency room and was diagnosed with high blood pressure. Learn how this Veteran took small steps to get and keep his blood pressure at a normal level. According to Danny, “if you want to live, you can do it.”
 Morris
Morris
Trained as a U.S. Army artillery gunner, Morris travelled many places during his military career after growing up in the small town of Brunson, South Carolina. As an adult, Morris experienced a four day headache that sent him to the emergency room. He learned he had high blood pressure. His heavy drinking made it difficult to control his blood pressure even with medication. Morris shares how the deaths of close family and friends made him stop drinking alcohol and change his eating habits. Now, he is known as the “food inspector” who helps those close him eat healthy.
 Patricia
Patricia
Patricia grew up in Chicago and joined the military along with two of her friends the year her mother died. Years later, she was diagnosed with high blood pressure. Patricia refused to take her medication because she did not like the side effects. A friend who ended up on kidney dialysis due to high blood pressure convinced Patricia to take her medication daily, as prescribed. Learn what Patricia does to manage her high blood pressure in addition to taking her medication.
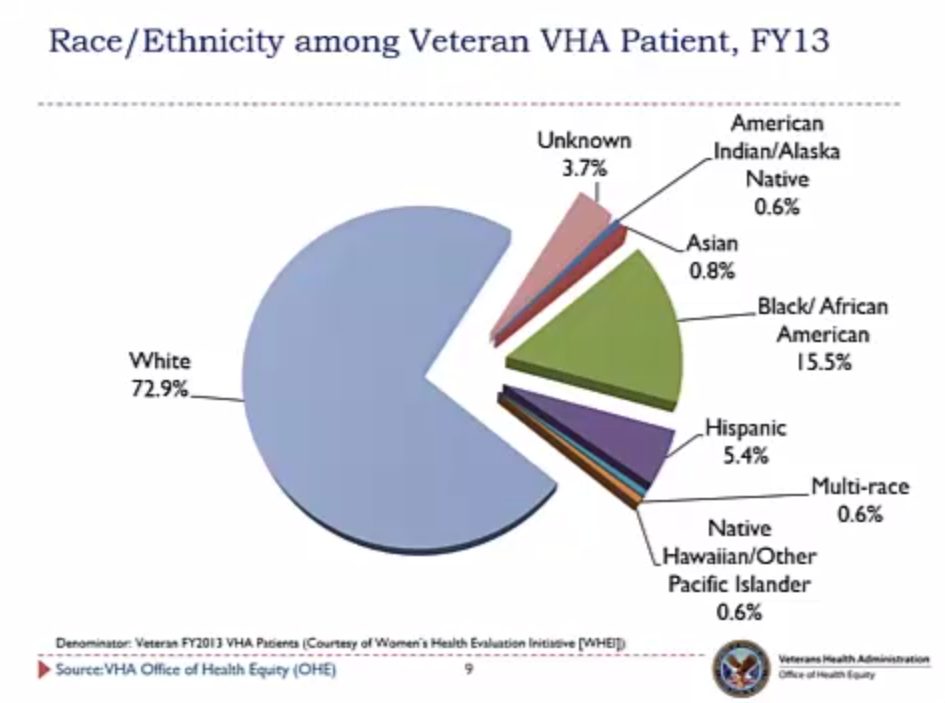
 The National Veteran Health Equity Report details patterns and provides comparative rates of health conditions for vulnerable Veteran groups. Specifically, this report is designed to provide basic comparative information on the sociodemographics, utilization patterns and rates of diagnosed health conditions among the groups over which the VHA Office of Health Equity (OHE) has responsibility with respect to monitoring, evaluating and acting on identified disparities in access, use, care, quality and outcomes. The report allows the VA, Veterans, and stakeholders to monitor the care vulnerable Veterans receive and set goals for improving their care.
The National Veteran Health Equity Report details patterns and provides comparative rates of health conditions for vulnerable Veteran groups. Specifically, this report is designed to provide basic comparative information on the sociodemographics, utilization patterns and rates of diagnosed health conditions among the groups over which the VHA Office of Health Equity (OHE) has responsibility with respect to monitoring, evaluating and acting on identified disparities in access, use, care, quality and outcomes. The report allows the VA, Veterans, and stakeholders to monitor the care vulnerable Veterans receive and set goals for improving their care.