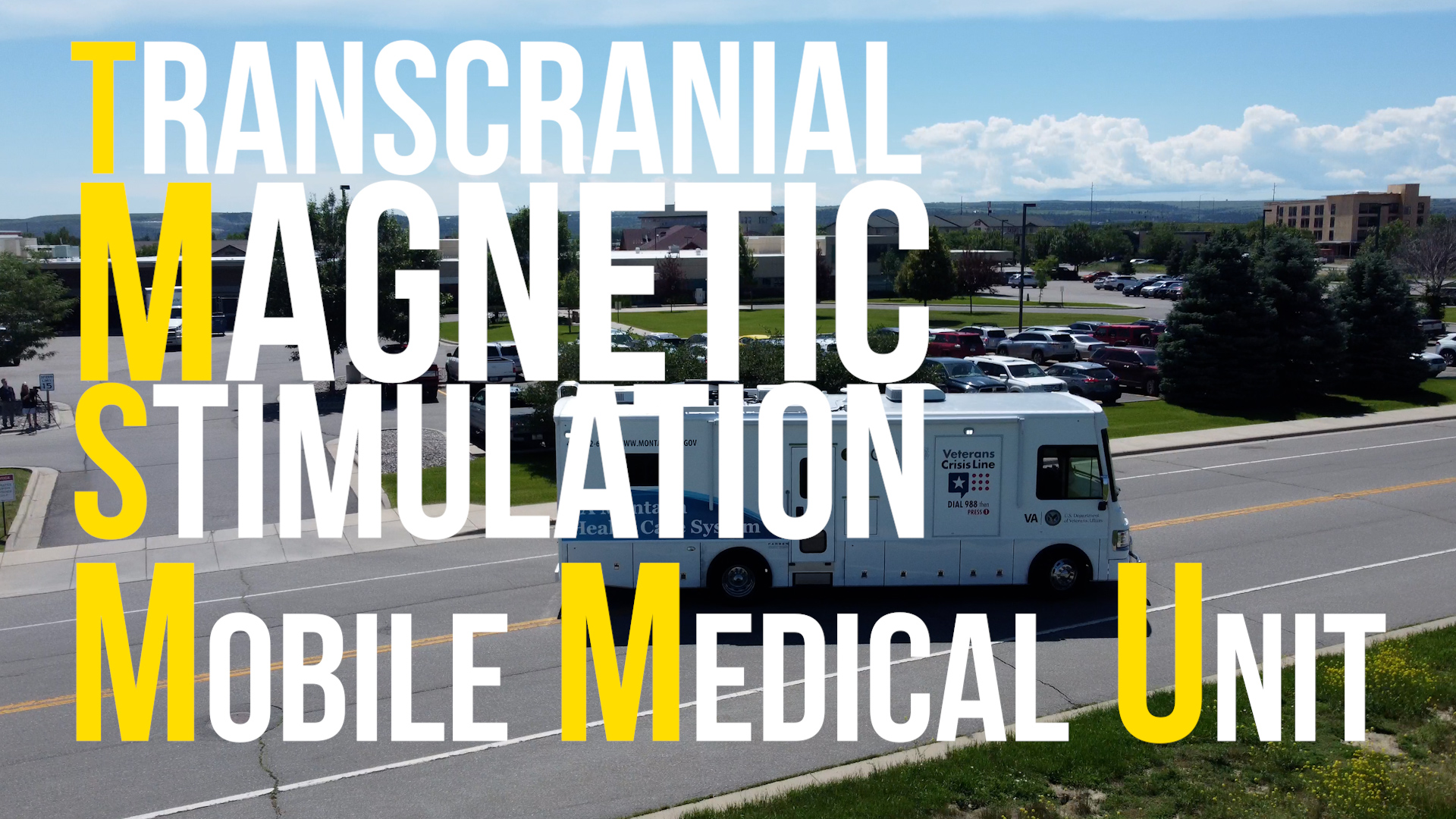
Transcranial Magnetic Stimulation (TMS) – Treatment for Depression
TMS therapy is an alternative treatment option for patients living with Major Depressive disorder (MDD) that have not achieved a satisfactory response to antidepressant medication. TMS uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression. TMS is safe, non-invasive and effective. TMS has been approved by the FDA since 2008 to treat depression. TMS is typically used when other depression treatments have not been effective.
What is Major Depressive Disorder (MDD)?
MDD is a disabling mental health condition characterized by feelings of sadness or despair, loss of interest in activities, changes in appetite, sleep and energy, and feelings of guilt or worthlessness. MDD can lead to trouble functioning at work or at home, and can contribute to suicidal thoughts.
How does TMS work?
During a TMS treatment session, an electromagnetic coil is placed against the scalp. The electromagnet delivers a pulse that stimulates nerve cells in a region of the brain that is involved in controlling mood. For depression we stimulate the “dorsolateral prefrontal cortex”, one of the major control centers of the brain. Stimulation of this region is thought to enhance its control of various symptoms of depression.
When is TMS used?
Antidepressant medications and psychotherapy are the first line treatments for major depression. These treatments, however, do not work for all patients. TMS is often used as an alternative option to assist with improving depression when medications and therapy have not adequately improved depression symptoms.
What happens during a TMS session?
Because TMS uses magnetic pulses, patients must remove any magnetic-sensitive objects (jewelry, hearing aids, credit cards) prior to treatment. Patients are required to wear earplugs during treatment for their
comfort and for hearing protection, as the TMS device produces a loud clicking noise with each pulse. Patients are seated in a comfortable chair and are awake for the entire session.
During the first session, several measurements are made to ensure the TMS coil will be properly positioned over the correct brain region. The TMS physician measures a “motor threshold” by administering several brief pulses over the left side of the brain. The motor threshold is the minimum amount of power necessary to make the patient’s thumb twitch, and this varies from person to person. Measuring the motor threshold helps the physician determine the correct amount of energy required to stimulate the brain.
Once the motor threshold is determined, the coil is placed directly over a brain region called the dorsolateral prefrontal cortex. This area is about the size of a golf ball and is located towards the front of the brain. Treatment is then started. During the treatment, the device taps on the scalp over this region. The patient can hear a series of clicking sounds and feel a strong tapping sensation on the scalp.
Who administers TMS?
TMS is prescribed and administered by a TMS-trained psychiatrist. The treatment team will also include a nurse or technician who will assist with treatment sessions.
How long is the procedure?
TMS occurs in a series of treatments. The treatments can vary in length from 3 minutes to 40 minutes, depending on the type of TMS utilized. A typical course of TMS includes at least 30 treatments. Depending on the number of treatments per day, the TMS protocol will last either 1 week or up to 6-8 weeks.
Do I need to be hospitalized to receive TMS?
No. TMS does not require any sedation or anesthesia. Patients are fully awake and aware during the treatment. There is no “recovery time” so patients can drive to and from the appointments and return to their usual activities as soon as the treatment is completed.
What are the side effects?
TMS is well tolerated and associated with very few side-effects. The most common side-effect (reported in about half of patients) is headaches. These are usually mild and diminish over the course of treatment.
About one-third of patients may experience painful scalp sensations or facial twitching with TMS pulses. These also tend to improve over the course of treatment. Adjustments can be made immediately in coil positioning to reduce discomfort.
The TMS device produces a loud clicking noise. Due to this earplugs are required during the treatment. There is no evidence to suggest permanent changes to hearing if earplugs are worn during treatment.
The most serious risk of TMS is seizures. However the actual risk of a seizure occurring during TMS is exceedingly low. At Montana VA Health Care System, we follow up-to-date safety guidelines that are designed to minimize the risk of seizures.
Who cannot get TMS therapy?
Patients with any type of non-removable metal in their heads (with exception of braces or dental fillings). Failure to follow this rule could cause the metal object to heat up, move or malfunction resulting in serious injury or death.
How to access care?
TMS is one of the alternative options for the treatment of depression offered at Montana VA Health Care System. The first step is to discuss the possibility of TMS with your mental health or primary care provider. Your provider will submit a consultation request to our clinic and one of our staff members will contact you for an in-person (or video-based) consultation. During your initial consultation, a thorough medical and mental health history will be taken, to determine if TMS might be safe and appropriate for you. We will also provide detailed information about TMS, including the treatment process, risks, benefits and side effects. At that time we will be able to answer any questions you might have, prior to you determining if you would like to proceed with treatment.
Want to learn more?
VA Montana Health Care System TMS Program
Scan codes below for more on TMS

Montana VA Transcranial Magnetic Stimulation (TMS) – Treatment for Depression Website

VA Palo Alto's Precision Neuromodulation Clinic

Veterans with PTSD Treated with Transcranial Magnetic Stimulation

Transcranial Magnetic Stimulation Video
Clinical Outcomes
TMS has been shown in large, controlled studies to be consistently effective in treating treatment-resistant depression. This means it often works for patients who have not previously responded to antidepressant medications. The following results were obtained from treating more than 800 veterans with treatment-resistant depression with TMS at outpatient VA clinics across the country.
What our veterans are saying about their treatment experience
- “I have not felt this good in many years.”
- “I felt like I was coming out of a coma and waking up again.”
- “It felt like each session another layer of dirt (depression) was being lifted off of me.”
Veterans Crisis Line
VETERANS CRISIS LINE: Dial 988 if you are experiencing suicidal thoughts or an acute mental health crisis (use logo with older male and younger female photo)
VA Montana Treatment Team
- Elizabeth Walter, M.D. – TMS Director
- Sean Bordelon, M.D. – TMS Psychiatrist (Remote)
- Gilbert Esser, M.D. – TMS Psychiatrist
- John Gillmore, M.D.- TMS Psychiatrist
- Emily McMillan, M.D – TMS Psychiatrist
- Nicholle Peralta, M.D. – TMS Psychiatrist (Remote)
- Russ Biddle, RN – TMS Nurse (Helena)
- Shae Lafuze, RN – TMS Nurse (Billings, MMU)
- James Simpach, RN – TMS Nurse (Kalispell)
- Shari St John, RN – TMS Nurse (Billings/MMU)
- Mimi Timeus, RN – TMS Nurse (Billings)
