Multiple Sclerosis Centers of Excellence
Determination of Multiple Sclerosis Subtypes
Rebecca Spain, MD, MSPH -- Portland, OR
Categorizing MS into clinical subtypes provides a common language to describe the variety of clinical courses of MS. Both prognosis and treatment differ based on clinical subtype. It also allows for more specific inclusion criteria in research studies; the more homogeneous the study population, the fewer patients are needed to demonstrate the benefits of a medication.
1996 MS Subtypes Consensus
A 1996 consensus of MS specialists identified and defined four MS subtypes: relapsing-remitting (RRMS), secondary-progressive (SPMS), primary-progressive (PPMS), and progressive-relapsing (PRMS). These four subtypes guided MS research and clinical practice for many years.
Relapsing-Remitting MS (RRMS)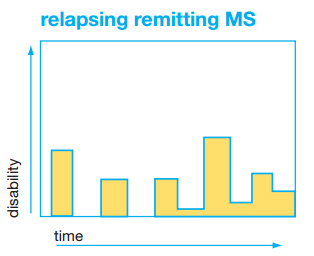
About 85% of people who are diagnosed have RRMS. RRMS is characterized by episodic exacerbations, or “attacks”, during which symptoms develop over a few days, remain for several weeks or months, and then resolve either completely or partially. If residual symptoms remain, they remain stable until the next exacerbation. The MRI in this subtype tends to show new lesions with and between exacerbations. It is estimated that about 10-15% of people with RRMS never transition to SPMS.
Secondary-Progressive MS (SPMS)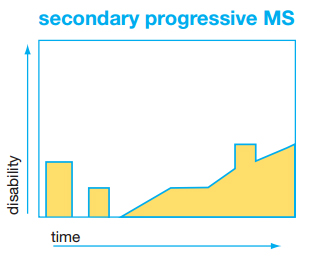
Most people with RRMS transition to SPMS after an average of 10- 20 years after diagnosis. In SPMS, there is gradual worsening of MS signs/symptoms between relapses. In most, relapses disappear altogether, but neurological disability continues to increase. The progression, while gradual, can have plateaus and may eventually stop worsening, or may continue to deteriorate over time. The MRI shows fewer new lesions and eventually no new lesions are seen despite ongoing clinical deterioration. It is thought that a different pathophysiology is driving SPMS than RRMS.
Primary-Progressive MS (PPMS)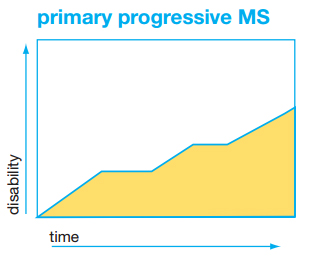
A smaller percentage of patients, 15% or less, do not ever experience acute relapses. Rather, these people experience disability progression from the onset without any distinct relapses or remissions. The MRI can show new lesion formation over time, but usually less so than RRMS, and new lesions may stop forming over time. There is debate whether the pathophysiology of PPMS and SPMS are the same or not.
Progressive-Relapsing MS (PRMS)
The PRMS subtype describes patients with both relapses and clear progression of disease dysfunction from the onset of PRMS. In the proposed descriptors by Lublin et al (below), this category is eliminated as it is a confusing term that may simply have indicated a more aggressive course of relapsing disease.
Although these terms are still used, the somewhat rigid definitions do not fully reflect our actual patient populations and can lead to confusion about treatment approaches.
2014 Proposed MS Subtypes Consensus
Proposed change in MS subtypes by Lublin et al. (2014) changes the framework to consider clinical courses as Relapsing MS or Progressive MS, and to think of the current stability of disease. Thus “Active” describes relapses (clinical relapses and/or MRI activity) and “Progression” describes clinical deterioration. Both SPMS and PPMS fall into the category of Progressive MS. The minimum period of time of evaluation is 1 year.
Relapsing MS
- Active (with relapses and/or new lesions on MRI)
- Not active (no relapses or MRI activity)
Progressive MS (SPMS and PPMS)
- Active with progression (relapses/MRI activity and clinical deterioration not due to relapses)
- Active but without progression (relapses but no clinical deterioration)
- Not active but with progression
- Not active and without progression (stable disease)
2014 Proposed MS Subtypes and Treatment
The Lublin model more closely follows our treatment approach as MS disease modifying therapies are proven effective for RRMS can be useful for both relapsing MS and progressive MS as long as there is evidence of active disease. Furthermore, as therapies become available for the non-relapse component of progressive MS, this nomenclature will help identify those who might benefit from these treatments. One might consider not initiating therapy or even stopping therapy if a patient has had stable disease if progressive MS or no activity if relapsing MS for quite some time, however there is a paucity of data to guide this decision.
This framework is quite helpful to set reasonable expectations of MS disease modifying therapy; a relapsing therapy is expected to only reduce MS relapses; therefore, it should greatly benefit a relapsing MS patient whose risk of disability comes from relapses. It is of less benefit to a patient with progressive MS as it will reduce the relapses but not the clinical deterioration from the progressive component of their disease.
Newer clinical trials have favored use of the term “relapsing MS” in order to broaden the qualifying patients who would benefit from an MS therapy designed to treat relapses.
Studying progressive MS has been more difficult given the reduction in relapses and slow clinical decline in this phase. Previous studies that seemed to benefit SPMS likely helped those who entered the study with active disease (relapses). The Lublin et al. nomenclature may better define populations for progressive MS studies.
Predicting Disease Prognosis with MS Subtypes
Although patients are often concerned about which type of MS they might have, using subtypes for prognosis is limited. It should be emphasized that these terms are used primarily for descriptive purposes. A patient with RRMS may accumulate significant disability between relapses while a patient with very slowly progressive disease may remain with minimal disability. While there are some predictors of better and worse disease courses, the strength of the prediction is modest at best. In clinical practice, subtypes are best used to help determine the appropriate MS treatments, and for setting reasonable expectations for the utility of that treatment.
Additional Information
Disclaimer: Links are provided as a convenience and for informational purposes only. They do not constitute an endorsement or an approval by MSCoE of any of the products, services, or opinions of the organization. MSCoE bears no responsibility for the accuracy, legality, or content of the external site or for that of subsequent links. Contact the external site for answers to questions regarding its content.



















