Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
About Multiple Sclerosis
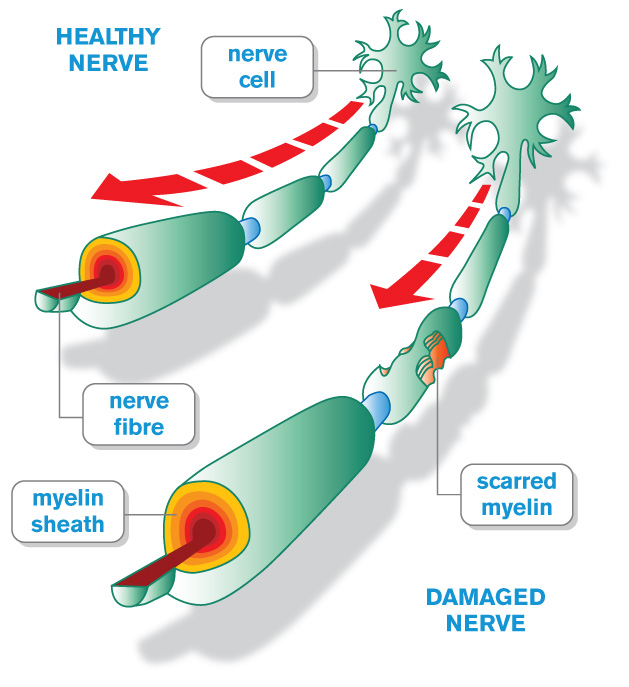 MS is a complex neurologic disease that affects the central nervous system (CNS) which includes the brain, spinal cord, and vision pathways. In MS, the immune system attacks the myelin sheath, the fatty tissue that surrounds and protects nerve fibers, as well as the nerve fibers themselves. This damage is called demyelination and the scar tissues that develop when myelin is damaged are called sclerosis, also known as lesions or plaques.
MS is a complex neurologic disease that affects the central nervous system (CNS) which includes the brain, spinal cord, and vision pathways. In MS, the immune system attacks the myelin sheath, the fatty tissue that surrounds and protects nerve fibers, as well as the nerve fibers themselves. This damage is called demyelination and the scar tissues that develop when myelin is damaged are called sclerosis, also known as lesions or plaques.
When any part of the myelin sheath or nerve fiber is damaged or destroyed, nerve impulses traveling to and from the brain and spinal cord are distorted or interrupted, causing a wide variety of symptoms. Sometimes the myelin can repair itself and the MS symptoms go away after the immune attack, or relapse. However over time, the myelin and underlying nerve fibers cannot recover and suffer permanent damage. This may lead to a decline in function depending on the disease course. Several MS disease courses have been identified.
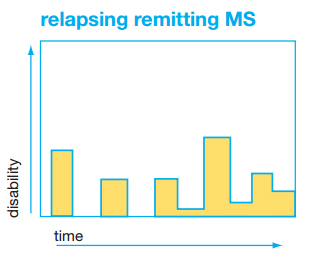 Relapsing-Remitting MS
Relapsing-Remitting MS
Relapsing-remitting MS (RRMS) is the most common MS disease course. About 85% of people with MS are first diagnosed with this course. It is characterized by clearly defined relapses. These relapses are followed by periods of partial or complete recovery with no apparent progression of the MS disability between relapses.
MS relapses, also called “attacks,” “exacerbations”, or “flares,” are rapid, significant worsening of existing symptoms or development of new symptoms, lasts at least 24 hours, and is not caused by infection, fever, or other stress. A relapse is different from the daily fluctuations in symptoms which are caused by variable function of the nervous system due to already existing MS plaques. In contrast to fluctuations, relapses are caused by new areas of inflammation and demyelination in the brain, spinal cord, or visual pathways. Most symptoms of relapses clear up with time, rest, and if needed, therapy. There are treatments that can speed up the rate of recovery from a relapse. However, if there is partial recovery, those remaining symptoms can become permanent. MS relapses typically last a few days to weeks. If not taking a disease modifying therapy, people with RRMS typically experience 1-3 relapses a year, however some can go decades between relapses.
Infection, fever, and stress can all lead to significant worsening of neurological function which can look like an MS relapse. This is called a pseudo-relapse because, like fluctuations, there is no new inflammation and demyelination occurring. A magnetic resonance image (MRI) can be helpful in distinguishing between MS relapses and pseudo-relapses. A pseudo-relapse is managed by treating the underlying infection or source of stress.
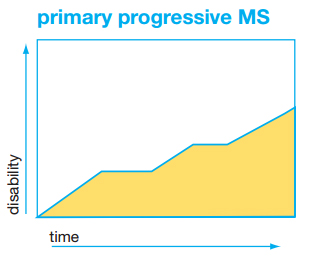 Primary Progressive MS
Primary Progressive MS
Primary progressive MS (PPMS) is characterized by progressive worsening of disease from onset without clear relapses. There may be changes in the rate of progression or periods of stability during the course of the disease. About 15% of people with MS are first diagnosed with this course.
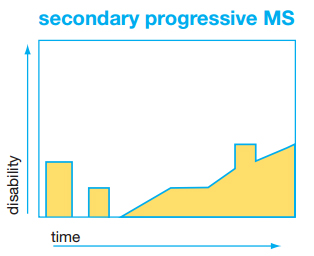
Secondary-Progressive MS
People with secondary-progressive MS (SPMS) are initially diagnosed with RRMS and then transition to this progressive form of the disease. This course is characterized by progression of disability over years, with fewer or no further relapses. In addition, there are fewer or no further new or enhancing plaques seen on the MRIs. Not everyone with RRMS will transition to SPMS.
Clinically Isolated Syndrome
Clinically isolated syndrome (CIS) is a term that describes an event similar to a typical MS relapse in a person not previously diagnosed with MS. People who experience a CIS are at higher risk of developing MS, but not all go on to have MS.
How is MS diagnosed?
The diagnosis of MS is complex. The symptoms and clinical signs of MS often come and go, and symptoms are not the same for every person. A diagnosis of MS is not based on one specific physical finding, laboratory test, or symptom, but rather the appropriate combination of findings, tests, and symptoms with the appropriate time course. The diagnosis of MS in some people is quite quick, taking a few weeks, when the person has a very typical presentation. It may take months or even years, when a person’s presentation is less typical.
To make a diagnosis of MS, a healthcare provider will complete a thorough evaluation of the person’s history and perform a physical examination. A magnetic resonance image (MRI) of the brain is almost always also required. Additional testing, including MRI of the spinal cord, spinal fluid analysis, and visual evoked potential tests, as well as repeated neurological examinations and imaging over time, may also be needed to definitively make the diagnosis of MS.
Although many of the symptoms cannot be seen on examination, there are specific guidelines that have been developed to help a healthcare provider (usually a neurologist) make the diagnosis of MS. For a person to be diagnosed with MS, the healthcare provider must:
- Find evidence of damage in at least two separate areas of the central nervous system (CNS), which includes the brain, spinal cord, and optic nerves. AND
- Find evidence that the damage occurred at least one month apart. Sometimes, spinal fluid abnormalities consistent with MS can be used to make this determination. AND
- ALSO, all other possible diagnoses must be ruled out.
Symptoms of MS often mimic those of other diseases. Ruling out any other condition is an important part of the diagnostic process. Although this may take time, it’s important that the proper diagnosis is given so that the best treatment options can be selected for the disease. The VA is committed to providing Veterans the specialized services and testing needed to establish an accurate diagnosis of MS.
What causes MS?
The cause of MS is currently unknown. What we do know suggests that there isn’t one single reason why someone gets MS. Instead, there are probably a number of different reasons, or factors involved - both genetic and environmental. There is a genetic link to MS, but it is not directly inherited like some other conditions. It isn’t caused by one faulty gene. Research into the genetics of MS has identified over 100 genetic variations that may play a role in MS. But not everyone who has these genetic variations will get MS. MS can occur more than once in a family. A parent, sibling, or child of someone with MS has a 1-4% chance of having MS. More distant relatives have a risk closer to that of the general population, which is 0.1-0.5% (1-2 people per one thousand people).
While there is a genetic element to MS, by no means is it the whole story. Several environmental factors have been identified. For instance, we know that MS is more common the further you are from the equator. This suggests there’s something in the environment related to distance from the equator that plays a role in MS. This something may be levels of vitamin D. Increasing evidence shows that low levels of vitamin D - before birth or during childhood - may increase someone’s chances of developing MS. Vitamin D is produced by our skin when exposed to sunlight. People who live closer to the equator tend to have more exposure to the sun.
Other research about environmental causes of MS shows that common childhood viruses, such as the Epstein Barr virus, may have a role to play in MS. Smoking and passive smoke-exposure increase the risk of developing MS. People with MS who smoke are more likely to experience worsening of their MS symptoms, progress to secondary-progressive MS at a faster rate, and have greater risk of increasing disability. It’s not yet clear exactly why this is, although one theory is that the chemicals in tobacco smoke affect the immune system. If you are a smoker, consider participating in the VA smoking cessation program. It’s healthier for you, and for others, especially children in your home. Finally, cardiovascular risk factors, like high blood pressure, high cholesterol, and diabetes, are all associated with worse outcomes in MS. It’s important for people with MS to reduce these risk factors with good diet, regular exercise, and close care with their primary care providers.
While some neurological diseases, such as amyotrophic lateral sclerosis (ALS), have been associated with deployment in the military, this relationship has not been seen with MS.
What are the symptoms of MS, and how can I manage them?
MS symptoms vary depending on the location of the plaques or lesions in the CNS. Lesions in the brain stem may cause double vision, a facial droop, facial pain, slurred speech, or imbalance. Lesions in a visual pathway can cause decreased vision in one eye. Spinal cord lesions can cause weakness, numbness, and/or bladder and bowel problems. Brain lesions can cause all of these symptoms as well as trouble with thinking, memory, and mood. Fatigue and pain are other very common symptoms of MS which can happen with lesions in any location.
Symptoms of MS are similar in all MS disease courses. Most people do not have all of the possible symptoms of MS, and no two people have the same combination or severity of symptoms.
How do I stop MS from getting worse?
There are now over a dozen MS disease modifying therapies that can slow the course of MS and reduce long-term disability. While most of these are for RRMS, treatments for PPMS and SPMS are emerging. Optimal care of MS includes a positive and active healthy lifestyle, a disease modifying therapy chosen with the guidance of an MS specialist, and the symptomatic therapies that meet the needs of the individual with MS.
Additional Information
- Combat-Related Chemical Exposure and the Link to MS and Other Neurological Diseases
- How to Decrease Your Children's Risk for MS If You Have MS
- Kurtzke Expanded Disability Status Scale (EDSS)
- Number of People in the U.S. with MS
- Understanding Your MRI Report
- National MS Society: What is MS?
- National MS Society: Diagnosing MS
- National MS Society: Possible MS
Disclaimer: Links are provided as a convenience and for informational purposes only. They do not constitute an endorsement or an approval by MSCoE of any of the products, services, or opinions of the organization. MSCoE bears no responsibility for the accuracy, legality, or content of the external site or for that of subsequent links. Contact the external site for answers to questions regarding its content.