Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
Pharmacy Requirements–Information for Providers
The information below identifies the requirements for prescribing medications to Veterans for prescription fulfillment services and pertains to medications prescribed under the Community Care Network (CCN).
Pharmacy Resources
Tool to find participating, in‑network retail pharmacies.
Pharmacy Benefits Management Services site including downloadable formulary files.
Resource to easily search for VA National formulary information.
On this page:
- Electronic Prescriptions
- Routine/Maintenance Prescriptions
- Urgent Care Prescriptions
- Filing a Pharmacy Claim
- VA Formulary
- Immunizations
Electronic Prescriptions (eRX)
The Department of Veteran Affairs (VA) now accepts electronic prescriptions from community providers for all eligible Veteran medications including controlled substances. Controlled substances include opioids, stimulants, and others.
VA will still accept and fill paper prescriptions (or fax where applicable); however, electronic prescriptions are recommended due to their ease and compliance with all state regulations.
NOTE:
- Use the published name of the VA pharmacy for e-prescribing. The published name is typically the town where the VA pharmacy is located, followed by "VAMC Pharmacy." For example "Buffalo VAMC Pharmacy."
- If you cannot electronically submit a prescription to a VA pharmacy, fax and hard copy prescriptions are accepted. Please contact the Community Care representative at the referring VA medical facility for the VAMC pharmacy fax number.
Routine/Maintenance Prescriptions
Routine/maintenance prescriptions must be sent to the referring VA medical facility’s pharmacy. If you do not have the ability to electronically submit prescriptions to pharmacies, please contact the Community Care representative at the referring VA medical facility for their pharmacy FAX number.
Prescriptions must generally be filled for no more than a maximum three-month (90-day) supply of medication. However, exceptions can be made for non-controlled medications and supplies to avoid breaking commercial package size, and for oral contraceptives if requested by the Veteran and their provider.
No prescription may exceed 12 months of therapy (including refills). For some prescriptions, a one-month (30 days) or less limitation may be established; these include controlled substances or any agent with a restriction not to exceed 30 days as specified by the VA National Formulary.
The following information must be included for the referring VA medical facility pharmacy to fill the prescription:
Patient Information
- Full patient name
- Patient address
- Date of birth
- Gender
- Patient phone number
- Social Security Number (Optional)
- Drug allergies
Provider Information
- Provider full name, address, phone and fax number
- Provider personal Drug Enforcement Agency (DEA) number (NOT facility-specific DEA number)
- Provider National Provider Identifier (NPI) number
Urgent Care Prescriptions
Medications that are needed immediately can be sent to an in-network retail pharmacy or VA pharmacy. If choosing a retail pharmacy, ensure the medication is on the VA Urgent Emergent Formulary by using the VA Formulary Advisor to perform a search.
NOTE:
- Up to a 14-day supply with no refills of the urgent care medication may be authorized
- Prescriptions can be filled at an in-network pharmacy, at VA, or at a non-network pharmacy. If a non-network pharmacy is used, Veterans must pay for the prescription and then file a claim for reimbursement with their local VA medical facility.
- If more than a 14-day supply of the medication is needed, the prescription must be sent to the referring VA medical facility pharmacy for fulfillment.
- A seven-day maximum supply for opioids, or up to the opioid prescribing limit allowed by state law — whichever is less — is authorized.
- Only eligible Veterans can use this benefit. The urgent care benefit is nontransferable and does not extend to family members.
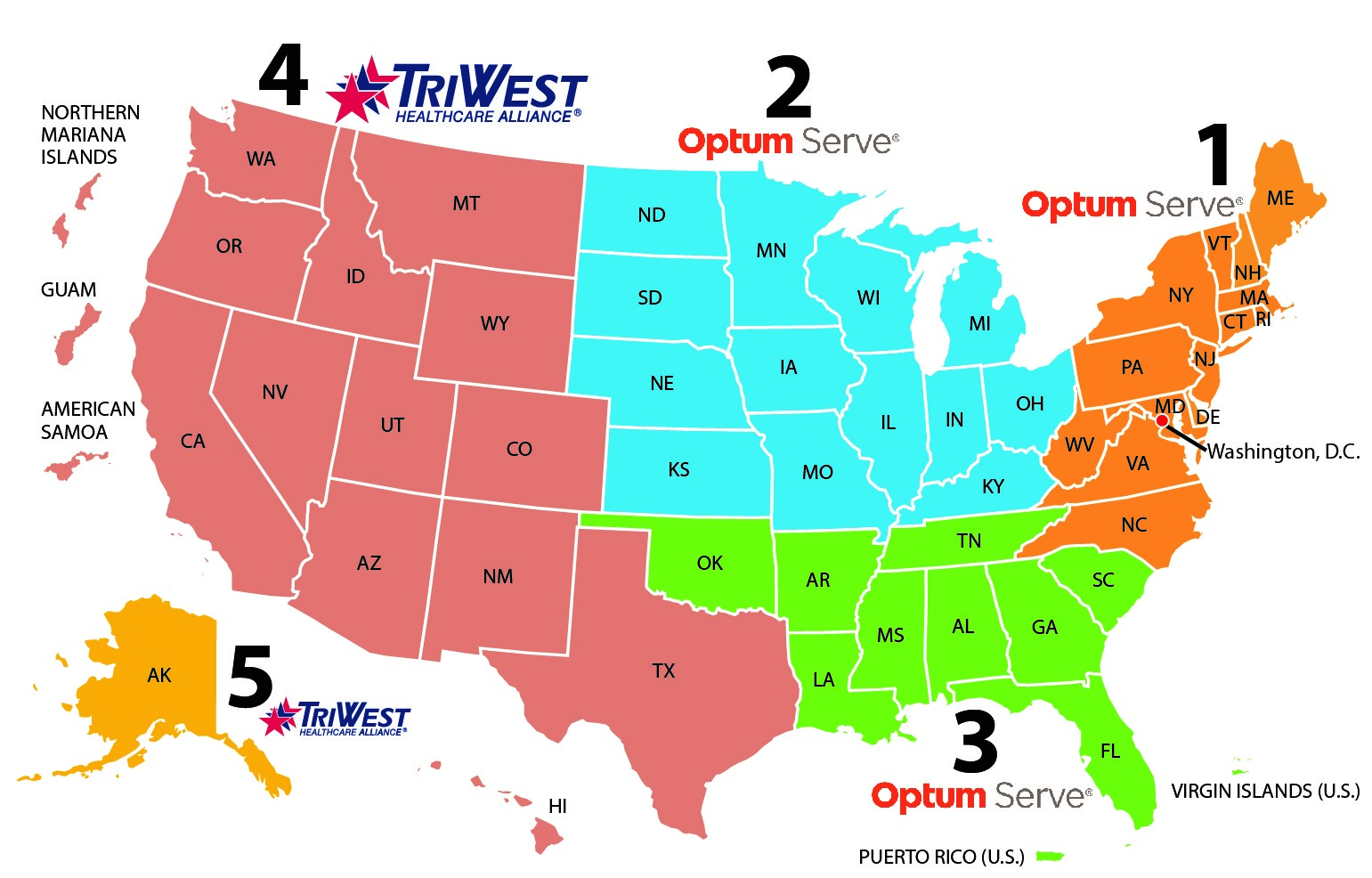
The Veteran must fill their urgent care prescription in the same state as their urgent care visit to avoid any issues. For a list of participating retail pharmacies, please use the VA Facility Locator. For telephone assistance finding an in-network, in-state pharmacy, contact the third party administrator that manages the region.
For Regions 1-3, contact Optum: 888-901-6609
For Regions 4-5, contact TriWest: 866-620-2071
Frequently Asked Questions about Prescribing Medications
How do I determine which pharmacy to send a prescription for fulfillment (VA or retail)?
Medications needed urgently can be sent to an in-network retail pharmacy or VA pharmacy. Urgent care prescriptions are listed on the VA Urgent/Emergent Formulary.
Routine/maintenance prescriptions must be sent to the referring VA medical facility’s pharmacy. If you do not have the ability to electronically submit prescriptions to pharmacies, please contact the Community Care representative at the referring VA medical facility for their pharmacy FAX number.
Does VA allow me to provide drug samples or coupons to Veterans?
No. The use of drug samples or drug coupons is prohibited.
Filing a Pharmacy Claim
For Regions 1-3 Pharmacies (Optum/CVS Caremark Pharmacy Network), enter VA pharmacy claims using the following steps:
- Enter BIN: 004336
- Enter PCN: ADV
- Enter Rx Group: RX4136
- Enter 10-digit Veteran ID*
- Enter Veteran’s date of birth (YYMMDD format)
For questions, please call the CVS Caremark Pharmacy Help Desk:
800-364-6331, 24 hours/7 days a week
For Regions 4-5 Pharmacies (TriWest/Express Scripts Pharmacy Network), enter VA pharmacy claims using the following steps:
- Enter BIN: 003858
- Person Code: 01
- Enter PCN: A4
- Enter Rx Group: VAPC3RX
- Enter 10-digit Veteran ID*
- Enter Veteran’s date of birth (YYYYMMDD format)
For questions, please call the Express Scripts Pharmacy Help Desk:
800-922-1557, 24 hours/7 days a week
*NOTE: If the Veteran does not have their 10-digit Veteran ID, please use the patient's 9-digit Social Security number and call the on-site assistance line.
On-site assistance line: 888-901-6609, Monday–Friday, 7 a.m.–10 p.m. ET
For more information, please review the Billing Information Card by scanning or clicking the QR code.
VA Formulary
The VA Formulary for Community Care is a comprehensive list of all medications listed alphabetically by generic name and can be found on the Pharmacy Benefits Management Services website. This site includes downloadable files for the VA National Formulary, VA Urgent/Emergent Formulary, and a searchable VA Formulary Advisor tool.
- The VA National Formulary indicates if a drug has a Criteria for Use (i.e., prior authorization), restrictions, or is listed on the Urgent/Emergent Formulary. Both the VA National Formulary and the VA Urgent/Emergent Formulary are updated regularly.
- The VA Formulary Advisor helps VA and non-VA users easily search for formulary items. Use the VA Formulary Advisor to search for a particular medication and determine if it is covered.
Frequently Asked Questions about Formulary
How do I request a medication from VA that has a criteria for use or is non-formulary?
All providers must follow the Veterans Health Administration (VHA) Directive 1108.08, VHA Formulary Management Process, including provisions for requesting medications with Criteria for Use. Criteria for Use can be found by searching for the medication in the VA Formulary Advisor and downloading the appropriate PDF if applicable.
Criteria for Use documents must be completed and submitted to the referring VA medical facility for review. If you need to submit a Criteria for Use document or non-formulary request for a medication, please contact the Community Care representative at the referring VA medical facility to obtain VA pharmacy contact information.
Community providers are encouraged to communicate results of prior authorization denials to the Veteran and determine appropriate next steps.
How do I request a non-formulary or prior authorization medication at a VA pharmacy?
All providers must follow the Veterans Health Administration (VHA) Directive 1108.08, VHA Formulary Management Process, which includes provisions for requesting non-formulary drugs. If you need to submit a non-formulary request for a medication, please contact the Community Care representative at the referring VA medical facility to obtain their non-formulary request form.
Can I request medications not on the Urgent/Emergent formulary at in-network retail pharmacies?
All medications that are not on the urgent/emergent formulary must be sent to a VA pharmacy for processing.
Immunizations
Free Flu Shot
Eligible Veterans can get a No-Cost Flu Shot from a nearby VA facility or an authorized community care location during flu season. Please refer to the VA Locator for authorized locations. For more information about billing, visit the Flu Vaccine Billing–Information for Providers page.
Flu Vaccine Billing – Information for Providers
COVID-19 Vaccinations
Eligible Veterans can get a No-Cost Covid-19 Shot from a nearby VA facility or an authorized community care location. Please refer to the VA Locator for authorized locations. For more information, visit the COVID-19 Guidance for Community Providers page.
COVID-19 Guidance for Community Providers
Other Adult Immunizations
Eligible Veterans with an existing approved community care referral are authorized to receive VA approved vaccines (Tdap, Shingrix, RSV and Pneumococcal) at in-network retail pharmacies. A prescription is required for all adult immunizations.
If a Veteran needs one of the VA approved adult immunizations, community care providers should send a prescription for the vaccine directly to an in-network, retail pharmacy for administration. If the Veteran does not have a community care referral, have them contact their local VA medical facility for additional guidance.
Process for Administering Adult Immunizations
Once it has been established that a Veteran requires a vaccine prescription (ONLY Tdap, zoster, pneumococcal, and RSV), VA providers should follow existing internal processes to obtain these vaccinations for Veterans. .
For community providers, please follow the steps below:
- Ask the Veteran for their preferred pharmacy. Ensure the pharmacy is in‑network. You can use the VA Locator to confirm the Veteran’s preferred pharmacy is in network.
- Ensure the medication is on the Urgent/Emergent Formulary. You can use the VA Formulary Advisor to search for the medication.
- Send a prescription to the pharmacy or provide the Veteran with a paper prescription.
- Inform the Veteran to bring the billing information to the pharmacy.
For more information, please review the Billing Information Card.


































