Urgent Care–Information for Providers
VA offers urgent care services to eligible Veterans at in-network urgent care clinics to treat minor injuries and illnesses that are not life-threatening, such as colds, strep throat, sprained muscles, and skin and ear infections.
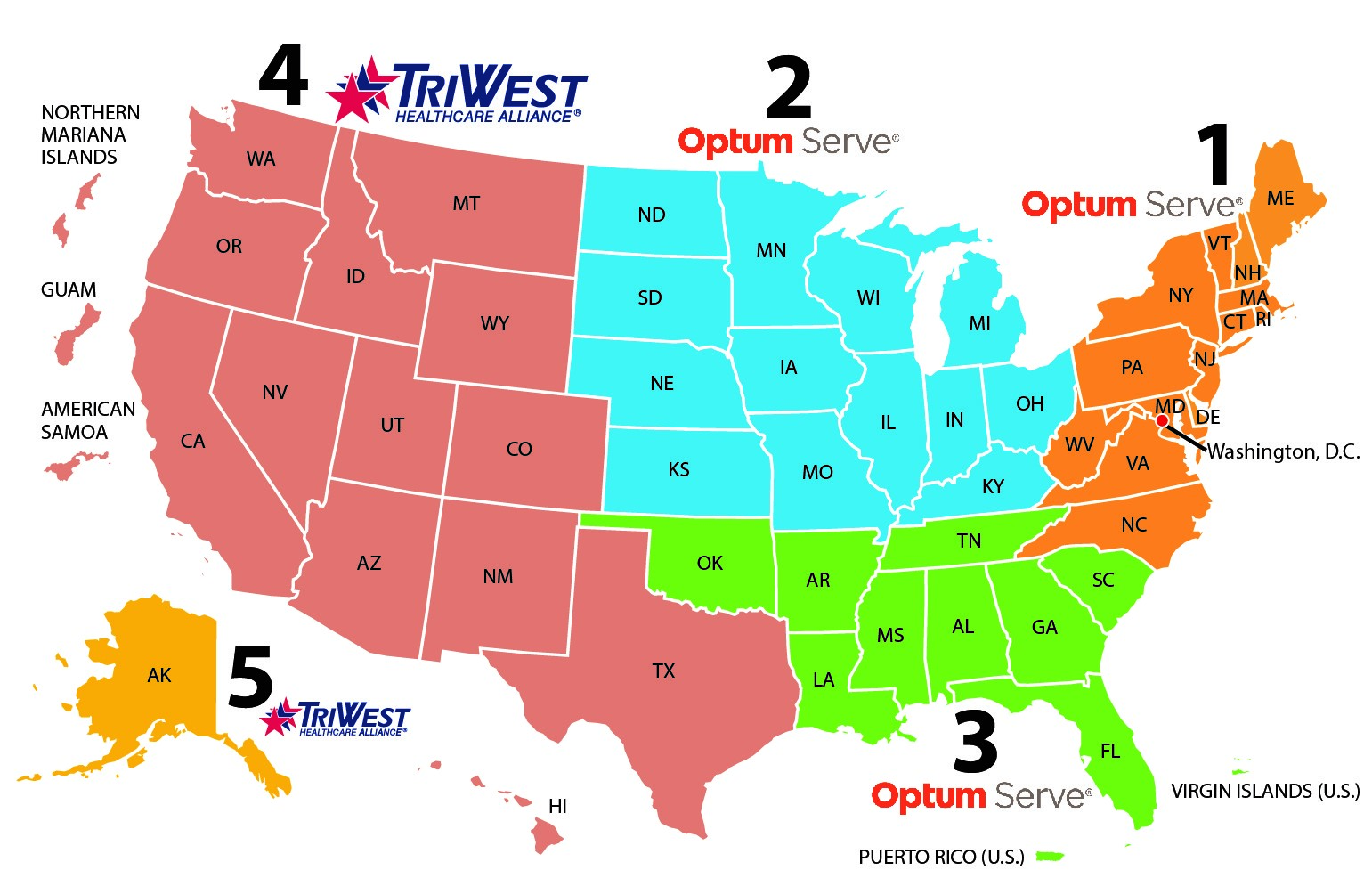
To serve Veterans under this benefit, you must be an in-network urgent care provider through a VA third party administrator (TPA). Optum is the TPA for Regions 1-3, and TriWest is the TPA for Regions 4-5.
For Regions 4-5, contact TriWest:
Community Care Network Region Map
Intake and Checking Eligibility
When a Veteran presents at an urgent care provider, you must check their eligibility for the urgent care benefit (this also activates their pharmacy benefit).
Check the Veteran’s eligibility by calling:
- For Regions 1-3: Contact Optum at 888-901-6609
- For Regions 4-5: Contact TriWest at 833-4VETNOW (833-483-8669)
Facility Contact Numbers for Care Coordination
Please use this list if you need to contact a VA medical facility to obtain additional clinical information.
DO NOT charge the Veteran a copayment. Copayment charges are billed separately by VA as part of the VA billing process.
Covered Services
To encourage eligible Veterans to seek care when and where they need it, VA does not publish a specific list of covered services for urgent care. However, VA excludes preventive and dental services, as well as other items that are not included in the medical benefits package, from the urgent care benefit. Contact the TPA assigned to your region for more information.
Care Coordination
Submit medical documentation within 30 calendar days to the Veteran’s home VA medical center (VAMC) via an approved method, such as Veterans Health Information Exchange (VHIE) or fax. Please also notify VA about any clinical concern needing follow-up.
Using the ZIP code of the Veteran’s residence, find the appropriate VA medical facility using the VA Facility Locator. Once the VA medical facility is determined, find the appropriate VA contact by using the Facility Contact Numbers for Care Coordination.
Prescribing Urgent Care Medication
For more information on prescribing urgent care medication, visit the Pharmacy Requirements–Information for Providers page.
Filing an Urgent Care Claim
After providing urgent care to a Veteran, the in-network urgent care provider must file a claim within 180 calendar days with the TPA assigned to their region. The TPA will adjudicate and pay claims on behalf of VA.
Instructions for Regions 1-3 Urgent Care Providers (Optum)
For urgent care providers in AL, AR, CT, DC, DE, FL, GA, IA, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MS, NC, ND, NE, NH, NJ, NY, OH, OK, PA, PR, RI, SC, SD, TN, VA, VI, VT, WI, WV
- Regional Support:
- Region 1: Call 888-901-7407 (M-F, 8:00 a.m. – 6:00 p.m. ET, excluding federal holidays)
- Region 2: Call 844-839-6108 (M-F, 8:00 a.m. – 6:00 p.m. ET, excluding federal holidays)
- Region 3: Call 888-901-6613 (M-F, 8:00 a.m. – 6:00 p.m. ET, excluding federal holidays)
- Electronic claims:
- Use Payer ID "VACCN" or
- Visit the secure Optum Provider Portal. Select “I am a Provider,” and then select "Medical/Behavioral Provider."
- Paper claims:
- Mail to VA CCN Claims–MEDICAL, P.O. Box 202117, Florence SC 29502
- Fax to 833-376-3047
Instructions for Regions 4-5 Urgent Care Providers (TriWest)
For urgent care providers in AK, AS, AZ, CA, CO, GU, HI, ID, MP, MT, NM, NV, OR, TX, UT, WA, WY
TriWest will adjudicate and pay claims on behalf of VA.
- Regional Support: Call 877-226-8749 (8:00 a.m. – 4:30 p.m. CT)
- Electronic claims: Enroll for electronic transactions on Availity.com. Go to TriWest Claims Information for more details.
- Paper claims:
- Mail to TriWest VA CCN Claims, P.O. Box 108851, Florence, SC 29502-8851
Filing a Pharmacy Claim
For more information on filing a pharmacy claim, visit the Pharmacy Requirements–Information for Providers page.
Frequently Asked Questions
Can the urgent care benefit be used by a Veteran’s family member?
Only eligible Veterans can use this benefit. The urgent care benefit does not extend to family members and is nontransferable.
How many times may a Veteran use the urgent care benefit in a calendar year?
There is no limit to the number of times a Veteran can access urgent care.
Contact Us
To confirm a Veteran’s eligibility for urgent care services, call:
- 888-901-6609 if located in AL, AR, CT, DC, DE, FL, GA, IA, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MS, NC, ND, NE, NH, NJ, NY, OH, OK, PA, PR, RI, SC, SD, TN, VA, VI, VT, WI, WV
- 833-4VETNOW (833-483-8669) if located in AK, AS, AZ, CA, CO, GU, HI, ID, MP, MT, NM, NV, OR, TX, UT, WA, WY
Resources
For general support, call the appropriate phone number listed below:
| Group | Regions 1-3 | Regions 4-5 |
|---|---|---|
| Providers | 888-901-6609 | 833-483-8669 |
| Pharmacists | 888-901-6609 (Optum) 800-364-6331 (Caremark) |
866-620-2071 (Urgent Care Support) 800-922-1557 (Express Scripts) |
| Veterans (Eligibility and general questions about the benefit) |
MyVA411 (800-698-2411) | MyVA411 (800-698-2411) |
| Veterans (Issues at the urgent care location) |
888-901-6609 | 866-620-2071 |